Angina Pectoris DefinitionAngina pectoris is a medical condition that is not limited to particular regions but is found in whole over the world. It is a type of chest pain that usually occurs when sufficient oxygen cannot reach the heart. This article will discuss what angina pectoris is, its causes, symptoms, diagnosis, treatment, and some case studies. 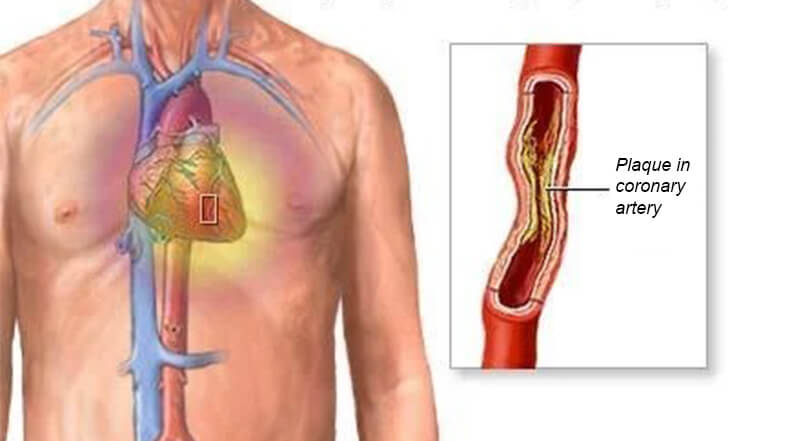
What is Angina Pectoris?Angina pectoris is when a person feels chest pain due to an insufficient supply of oxygen (in the form of oxygen-rich blood) to the heart. It is usually caused when the coronary arteries contract, which are the blood vessels that supply blood to the heart. This contracting is often due to plaque build-up on the inner walls of the arteries, a condition known as atherosclerosis. Causes of Angina PectorisAngina pectoris often occurs when blood flow to the heart is insufficient, usually due to contracting or jamming one or more coronary vessels. The coronary arteries are responsible for supplying oxygen-rich blood to the heart. The most common cause of angina pectoris is Coronary Artery Disease (CAD), which is caused when stuff or impurities starts collecting on the walls of the arteries from inside, which results in contracting and reducing the amount of blood flow to the heart. These impurities contain cholesterol, fat, and other substances ready to stick to the walls of the blood vessels and form a barrier in the blood flow. Other causes of angina pectoris may include:
Risk factors that increase the possibility of developing angina pectoris include:
It is important to note that angina pectoris can also be a warning sign of an upcoming heart attack. If you experience any symptoms of angina pectoris, it is advisable to seek medical attention immediately to rule out a more serious condition. There are three angina pectoris: Stable, Unstable, and Variant. 1. Stable AnginaThe most typical type of angina is stable angina pectoris, generally brought on by exercise or psychological strain. It is usually caused when the coronary arteries contract, which are the blood vessels that help transport blood to the heart. This narrowing is often caused when stuff or impurities starts collecting on the walls of the arteries from inside, which results in contracting and reducing the amount of blood flow to the heart. Symptoms of Stable Angina Pectoris Chest pain and difficulty breathing are the primary signs of stable angina pectoris. The chest pain is typically characterized by snugness, strain, and pressing. The pain occurs in the arms, legs, shoulders, neck, bite, or spine. Other symptoms of stable angina pectoris may include short duration of the breath, sweating, dizziness, fatigue, and palpitations. These symptoms usually occur during an outdoor activity or overthinking and are relieved by providing rest to the body and the mind. Diagnosis of Stable Angina Pectoris Physical examination and an evaluation of the patient's past medical conditions are usually the first steps in determining the existence of stable angina pectoris. Additionally, the doctor may request several procedures, including an electrocardiogram (ECG), a stress test, or a blood test. An ECG is a very helpful technique used in the medical field to spot various problems in the human heart. It is a particular test that captures the heart's electrical signals and can be used to find irregularities in the beat or architecture of the heart. During a stress test, the patient is monitored while exercising on a treadmill. High amounts of cholesterol, glucose, or specific enzymes released when the heart muscle gets injured can all be checked for using a blood test. Treatment of Stable Angina Pectoris The treatment of stable angina pectoris usually involves a mixture of lifestyle changes and medication. Lifestyle changes may include quitting smoking, losing weight, exercising regularly, and eating a healthy diet, low in saturated fat, trans fat, and cholesterol, avoiding eating out fast food very often. These changes can help reduce the risk of further impurity collection in the coronary arteries. Medications used to treat stable angina pectoris may include nitro-glycerine, which can help relieve chest pain by dilating the blood vessels and increasing blood flow to the heart. Other medications may include beta-blockers, calcium channel blockers, and nitrates. In some cases, surgery may be needed to treat stable angina pectoris. This may include procedures such as angioplasty, which involves using a small balloon to widen the narrowed artery, or coronary artery bypass surgery, which consists in creating a new blood vessel to bypass the blocked artery. This method is very risky in life. Overall, Stable angina pectoris is usually caused when the coronary arteries contract, the blood vessels that help transport blood to the heart. This narrowing is often caused when stuff or impurities starts collecting on the walls of the arteries. Chest pain and difficulty breathing are the primary signs of stable angina pectoris. An ECG is a very helpful technique used in the medical field to spot various problems in the human heart. The treatment of stable angina pectoris usually involves a mixture of lifestyle changes and medication. 2. Unstable AnginaUnstable angina pectoris is a type of angina that occurs suddenly and unpredictably, even at rest. Unlike stable angina, which is triggered by physical activity or emotional stress, unstable angina can occur at any time, including during periods of rest or sleep. Unstable angina is caused by an immediate and serious decrease in blood flow to the heart. This reduction in blood flow is typically due to the rupture of a plaque within one of the coronary arteries, which can cause the formation of a blood clot. Symptoms of Unstable Angina Pectoris The symptoms of unstable angina pectoris are like those of stable angina but are usually more severe and last longer. They may include:
Diagnosis of Unstable Angina Pectoris Physical examination and an evaluation of the patient's past medical conditions are usually the first steps in determining the existence of stable angina pectoris. Additionally, the doctor may request several procedures, including an electrocardiogram (ECG), a stress test, or a blood test. Blood tests can be used to check for high levels of cardiac enzymes released when the heart muscle is damaged. Imaging tests, such as a stress echocardiogram or a cardiac MRI, can be used to evaluate the function and structure of the heart. Treatment of Unstable Angina Pectoris The treatment of unstable angina pectoris aims to restore blood flow to the heart and prevent further complications. Treatment may include medications such as nitro-glycerine, aspirin, beta-blockers, or heparin, which can help reduce the formation of blood clots and relieve chest pain. Angioplasty involves using a small balloon to widen the narrowed artery, while coronary artery bypass surgery involves creating a new blood vessel to bypass the blocked artery. Overall, Unstable angina pectoris is a critical condition, and the person should be in regular touch with medical services to avoid further damage to life. It is characterized by sudden and unpredictable chest pain or discomfort, even at rest. Treatment may involve medications or more invasive procedures, depending on the situation. 3. Variant AnginaVariant Angina pectoris, also known as Prinz metal's angina, is a rare form of angina that occurs when the coronary arteries temporarily become stiff or constrict, reducing the amount of blood flow to the heart muscle. Unlike stable angina, typically initiated by over-physical activity or emotional stress, variant angina can occur when the body is at rest, usually during the night or early morning hours. The pain can be serious, and the period can be 40 minutes. Symptoms of Variant Angina Pectoris The symptoms of variant angina pectoris are similar to those of other anginas but occur at rest and can be more severe. Symptoms may include:
Diagnosis of Variant Angina Pectoris Physical examination and an evaluation of the patient's past medical conditions are usually the first steps in determining the existence of stable angina pectoris. Additionally, the doctor may request several procedures, including an electrocardiogram (ECG) and a stress test. An ECG can help detect changes or irregularities in the heart's contraction and relaxation, and coronary angiography can help identify any areas of the coronary arteries that are narrowed or blocked. A defined type of dye is injected into the blood vessels to notice the blood flow to the heart, and on this basis, the situation is identified. Treatment of Variant Angina Pectoris Treating variant angina pectoris typically involves medications to help relax the coronary arteries and prevent further spasms. These may include calcium channel blockers, nitrates, and long-acting nitrates. In some cases, more complicated techniques, such as angioplasty or stenting, are required to treat the blocked/ jammed arteries. So that the blood could easily flow through them and reach their destination, coronary artery bypass surgery may not be mandatory for some patients. Prevention of Variant Angina Pectoris To prevent future episodes of variant angina pectoris, patients should avoid triggers that may cause coronary artery spasms, such as exposure to cold temperatures, smoking, or using stimulants like cocaine or amphetamines, following a healthy routine, containing exercise daily, and consuming healthy food. Overall, Variant angina pectoris is a rare but serious condition that can cause severe chest cramps or irritation while the body rests. It is caused by constriction of the coronary arteries, which can decrease the amount of blood flow to the heart. Treatment may include medications or more invasive procedures, depending on the condition. Angina pectoris patients must be serious about treatment to avoid further critical conditions. Living a healthy lifestyle plays an important role in avoiding any critical condition like that of angina pectoris. What are Some of the Precautions That Can be Taken to Avoid Angina Pectoris?Several precautions can be taken to reduce the risk of developing angina pectoris. Some are given below:
In summary, taking steps to maintain a healthy lifestyle, managing medical conditions, managing stress, taking medications as prescribed, regular check-ups with your doctor, avoiding triggers, and following your treatment plan can help reduce the risk of developing angina pectoris. Case StudyNote: This case study is a hypothetical scenario created for educational purposes only and does not contain content based on real life.Patient Background Mrs. X, a 65-year-old woman, had a history of hypertension, diabetes, and high cholesterol. She was a homemaker and lived a lazy lifestyle with less physical activity. Mrs. X was under medical supervision and regularly took medication for her condition. Symptoms Mrs. X had complained of chest cramps and irritation for the past few months. She described the pain as a squeezing or tightness feeling in her chest, which would occur during physical exertion or stress. The pain would usually subside with rest, but it had become more frequent and severe in recent weeks. Medical Assessment Mrs. X's family doctor referred her to a cardiologist, who performed an electrocardiogram (ECG) and stress test. The results indicated that Mrs. X had angina pectoris, a medical condition caused by decreased blood flow to the heart muscle due to contraction or blocked blood vessels called coronary arteries. The cardiologist prescribed nitro-glycerine tablets be taken sublingually during an angina attack and advised Mrs. X to make amendments to her daily life routine, such as increasing physical activity and consuming a heart-healthy diet. Event One evening, Mrs. X experienced severe chest pain while sitting at home. She immediately took her nitro-glycerine tablet but did not feel any relief. She called her daughter, who lived nearby, for help. Mrs. X's daughter rushed her to the hospital, but Mrs. X collapsed in the car and was unresponsive when they arrived at the emergency department. Outcome Despite immediate resuscitation efforts, Mrs. X was pronounced dead on arrival. An autopsy revealed that she had suffered a massive heart attack due to a complete blockage of one of her coronary arteries. The blockage had likely been building up over time, leading to chronic ischemia and angina pectoris. The sudden rupture of a plaque in the artery had caused a blood clot to form, leading to a complete occlusion of the vessel and subsequent heart muscle damage. Mrs. X's sedentary lifestyle, underlying medical conditions, and delayed medical intervention contributed to the development and progression of her coronary artery disease. Conclusion Angina pectoris is a warning sign of underlying coronary artery disease and requires prompt medical attention. Patients with risk factors for heart disease, such as hypertension, diabetes, and high cholesterol, should undergo regular cardiac assessments and make lifestyle changes to prevent or manage the condition. Failure to do so can lead to serious consequences, such as heart attack and sudden death. Case Study 2Here is another hypothetical case study: Patient Background Mr. Y, a 42-year-old man, had a history of smoking, high blood pressure, and a family history of heart disease. Despite his doctor's recommendations, he worked a high-stress job and often neglected his health. Mr. Y did not exercise regularly and had a poor diet, often consuming fast food and processed snacks. Symptoms Mr. Y had been experiencing chest pain and breathing difficulty for several days. He initially dismissed the symptoms as indigestion or stress but noticed that the pain was not going away and seemed to worsen. He also felt tired and lightheaded. Medical Assessment Mr. Y's wife convinced him to see a doctor, who performed an electrocardiogram (ECG) and blood tests. The ECG showed signs of a heart attack, and the blood tests confirmed elevated levels of cardiac enzymes, indicating heart muscle damage. Mr. Y was immediately taken to the cardiac catheterization facility for additional testing and care. Event During the cardiac catheterization procedure, the cardiologist discovered that Mr. Y had a blockage in one of his coronary arteries. The blockage was severe, and the cardiologist decided to perform an emergency angioplasty and stent to restore blood flow to the heart muscle. The procedure was successful, and Mr. Y was transferred to the cardiac intensive care unit for post-operative care. Outcome Despite the successful angioplasty, Mr. Y's condition remained unstable, and he developed complications, including heart failure and arrhythmias. The medical staff's tireless efforts steadied his health, but Mr. Y's heart function deteriorated. Sadly, Mr. Y died three days after the procedure due to a massive heart attack. Conclusion Mr. Y's case highlights the importance of recognizing and addressing the risk factors for heart disease, such as not engaging in physical activities, poor eating habits, etc. Patients with heart attack symptoms, such as chest pain and shortness of breath, should seek immediate medical attention to minimize the damage to the heart muscle and improve their chances of survival. Living a healthy lifestyle plays an important role in avoiding any critical condition like that of angina pectoris.
Next TopicAverage Definition
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share