Basal Ganglia CalcificationGanglia calcification is also known as Fahr's disease and sometimes called as familial idiopathic basal ganglia calcification. It is an exceedingly rare neurodegenerative disease which is characterised by calcifications in the basal ganglia and other parts of the brain. The basal ganglia calcification might be asymptomatic or linked to neuropsychiatric and motor symptoms. 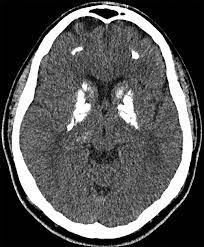
Fahr's disease or Basal Ganglia CalcificationFahr's disease is a very much rare neurological situations which is marked by symmetrical and bilateral basal ganglia calcification, and it is caused by familial idiopathic basal ganglia calcification. Other brain parts may also calcify, including the cerebral cortex, thalamus, and dentate nucleus. Fahr's illness has been reported in familial and nonfamilial cases, primarily in an autosomal-dominant manner. There are numerous clinical manifestations of the disease, most of which have neuropsychiatric characteristics and mobility abnormalities. Cognitive impairment, depression, delusions, hallucinations, anxiety, manic symptoms, schizophrenia-like psychosis, and personality change are some of the psychiatric characteristics or symptoms of this rare disease. Some of the Clinical symptoms of basal ganglia calcification include parkinsonism, ataxia, headache, seizures, vertigo, stroke-like episodes, orthostatic hypotension, tremor, dysarthria, and paresis. Fahr's illness should be considered when making a differential diagnosis of psychiatric symptoms, especially if a mobility disorder is present. It is essential to distinguish the disease from other illnesses resulting in cerebral calcification. Basal ganglia calcification is an incurable disease, there is no specific treatment available in medicine right now. More study is required to fill the gaps in our present understanding of the prevalence, aetiology, symptoms, and management of Fahr's disease. Numerous neurological and metabolic illnesses are linked to basal ganglia calcifications, and calcifications may also be a common incidental finding on neuroimaging in asymptomatic people. Basal ganglia calcification, to some extent, might be regarded as "natural" with ageing after the age of fifty and may be discovered by accident in 15-20% of asymptomatic patients having a computed tomography (CT) scan. Theodore Fahr was the first person to report brain calcifications. This condition is sometimes referred to as Fahr's or Fahr's syndrome (because of its scientist name). Fahr explained a case study of an 81-year-old patient who have a history of dementia and post-mortem evidence describe calcifications in the whitish matter, basal ganglia, and tiny cerebral arteries, which were be caused by aberrant calcium-phosphorus ratios. Delacour recorded the existence of vascular calcifications of the basal ganglia in a 57-year-old man who had stiffness, weakness, and tremor of the lower extremities in 1850 clinically. Then, in 1855, Bamberger characterised a woman with mental retardation and convulsions' calcifications in the thinner cerebral veins as a histological entity. Numerous terms have been used to refer to this condition over the years; the word "idiopathic basal ganglia calcification" (IBGC) was first used in 1974 when two cases of familial brain calcification of unknown origin that exhibited characteristics of "dystonia Musculo rum deformans" were reported. The term "bilateral striopallidodentate calcinosis (BSPDC)" has been used as a descriptive word since these calcifications frequently target the dentate nuclei and basal ganglia. "Primary familial brain calcification" (PFBC) is a term which was first used in 2013, it refers to a genetically proven neurodegenerative illness which involves the deposition of calcium in the basal ganglia and other areas of brain. More than one hundred kinship and sporadic cases have been documented, and utilising varying levels of pathogenicity evidence, population genomic data analysis estimates of the lowest incidence of PFBC ranged from 4.5/10000 - 3.3/1000. To differentiate between primary and secondary forms and account for the various anatomical distributions detected, the term "primary bilateral brain calcification" has only recently been proposed for inherited and sporadic instances. In numerous studies, doctors choose to keep PFBC as the key term which refers to both inherited and sporadic variants because of the relative novelty of this new nomenclature. In contrast, the term "syndrome" has been proposed when a secondary, potentially curable cause is discovered and has been connected to various ailments, particularly endocrine disorders. These circumstances result in metabolic dysfunctions that cause an aberrant calcium/phosphorus ratio, colloidal precipitation in cerebral arteries, and the composition of calcified deposits. Aetiology and PathophysiologyFahr's illness has been recorded in familial and nonfamilial cases, primarily in an autosomal-dominant manner. Fahr's disease has a location on chromosome 14q, according to a whole-genome analysis of 24 members of a multigenerational family with dominantly inherited idiopathic basal ganglia calcification. As an etiological component for both childhood and adult psychiatric diseases, including Asperger's syndrome and attention deficit hyperactivity disorder (ADHD), the relationship between calcium homeostasis and a disrupted blood-brain barrier has been proposed (such as schizophrenia, mood disorders, and anxiety disorders). The idea is supported by research showing that psychiatric illnesses may have altered calcium homeostasis, signalling, and dysregulation of calcium. A increase in neuronal calcium sensor-1 in the brain's dorsolateral prefrontal cortex is seen in the adult patients with bipolar and schizophrenia disorder. Fahr's disease patients' calcification is a mysterious phenomenon with no evident cause. Calcification may be caused by metastatic deposition, which develops due to local blood-brain barrier rupture, or it may be brought on by a problem with the calcium metabolism of neurons. In patients with Fahr's disease, homocarnosine, a peptide unique to the central nervous system, was 2-fold higher in the CSF analysis than in controls; in rare cases, homocarnosine was not detectable, and the histidine level was low. Some patients having Fahr's disease have a high level of copper, zinc, iron, and magnesium in their body. Basal ganglia perfusion to both sides of the brain's calcified regions was significantly reduced, as was cerebral cortex perfusion, according to an evaluation of regional cerebral blood flow to the calcified areas. Fahr's disease patients have shown reduced glucose metabolism in the basal ganglia and the frontal brain area, which may point to a frontostriatal circuit breakdown. According to a gross pathologic brain examination, the striatum, internal capsule, white matter, and cerebellum have granular material and solid nodules accumulates there. In small and medium-sized artery walls, concentric calcium deposits were visible histologically. Along with capillaries, droplet calcifications might be seen. If there is high calcium deposits then it may surround diffuse gliosis, and basal ganglia, cortical areas, and sub-cortical regions that experience ischemic alterations. Clinical features of Fahr's diseaseThe disease begins slowly and typically affects middle-aged patients with various neurological and psychological symptoms. Numerous different circumstances can lead to bilateral symmetric calcification. It may not have any signs or be linked to multiple clinical disorders, such as pseudo-hypoparathyroidism or neurological diseases. Fahr's condition must meet different types of criteria to be diagnosed which includes : evidence for the bilateral basal ganglia calcification; increasing neurological or neuropsychiatric manifestations; the onset of symptoms is typically in the fourth or fifth stage, though the earlier start is possible; there is no evidence from biochemical abnormalities and clinical features that suggests the presence of mitochondrial or metabolic disease or other systemic disorders, and the calcification is not caused by infection. Even in the absence of one of the first two criteria, a diagnosis can be made if there is a family history. Most reports of calcification come from the globus pallidus. The putamen, internal capsule, dentate nucleus, thalamus, cerebellum, and cerebral whitish matter are some different type of the additional sites of calcification that have been reported by doctors. Numerous cases were unintentionally diagnosed while being evaluated for other medical or psychiatric conditions. This calls into question the disease's rarity and raises the likelihood that cases of Fahr's disease may not have been adequately reported. SymptomsCranio-cerebral trauma, stroke, meningitis, encephalitis, brain tumours, cerebral aneurysms, arterio-venous malformations, subdural hematomas, and mastoiditis are additional clinical findings in Fahr's disease patients. Fahr's disease and abnormal calcium metabolism were present in many different cases, and idiopathic hypoparathyroidism, hyperparathyroidism, pseudo-hypoparathyroidism, and postoperative hypoparathyroidism were also found to be present in the patients. More severe mental impairment was observed in some other patients with parathyroid hormone deficits due to thyroidectomy. ConclusionWe concluded that the Fahr's disease is a very rare neurodegenerative condition marked by the dentate nucleus of the cerebellum and bilateral symmetrical basal ganglia calcifications. This state should be considered when making a differential diagnosis of psychiatric symptoms, whether the symptoms are acute or persistent. A brain CT scan may aid in an early diagnosis. Additional study is required to close the information gap regarding prevalence, aetiology, symptoms, and therapy.
Next TopicBasal Ganglia Function
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










