What is the full form of CHC1. CHC: Community Health CentersCHC stands for Community Health centers. A healthcare centre or community health center is one of a network of clinics staffed by general practitioners and nurses who offer medical care to residents of a particular area. The majority of individuals in nations with universal healthcare visit hospitals. The low-income residents of places with a limited permit to primary healthcare are among the clientele in countries without universal healthcare. More extensive medical facilities in Central and Eastern Europe are sometimes referred to as policlinics (not to be confused with polyclinics). 
The Community Health Centers is how CHC is formally referred to. CHCs are private, nonprofit organizations that deliver healthcare services in response to consumer involvement and influence. Community Health Centres also provide essential healthcare services for those in the area who lack access to primary healthcare. In central and eastern Europe, primary healthcare facilities are known as policlinics. Informational Nuggets Regarding CHCA network of general practitioners and nurses helps CHC by offering medical care to local populations in a particular area. The essential services given by CHCs include family practice and dental care. Still, some hospitals have significantly extended maternity care, pharmacy, birth control, optometry, laboratory analysis, pediatrics, internal medicine, women's health, and more. The Programme Evaluation Organization conducted the study at the request of the Planning Commission to assess the operation of Community Health Centres (CHCs) and their efficiency in bringing specialized healthcare to rural residents. 
Additionally, the Planning Commission's Health Division and the Department of Health and Family Welfare identified several specific challenges that the study required to address. Among them are evaluations of the following:
MethodologyWe must analyze secondary and primary data to examine the numerous hypotheses related to the study's aims. Most of the data needed for the study was gathered by a sample survey, while information from published sources was also obtained and used as needed. Consequently, they collected state and district-level statistics on health indicators and infrastructure from published papers. Still, information related to health care institutions (CHC/PHC) and household level data had to be generated through the PEO field units' gathering micro-level data. 
For the study, they used a multiple-stage sampling design. The first stage sample units are the eight states that purposefully chose to reflect both "excellent" and "bad" population health status. A stratification factor was the newborn mortality rate. For the study, four states with IMRs above the national average-Madhya Pradesh, Uttar Pradesh, Rajasthan, and Orissa-and four with IMRs below or equal to the national average-Tamil Nadu, Maharashtra, Bihar, and Haryana-were selected. Each state had two districts were chosen, one with a low IMR and the other with a high IMR. For each desired section, two CHCs-one close to and the other far from the district hospital-was chosen in the third stage. In the fourth sampling step, two PHCs covered by a CHC and eight patients (four indoor and four outdoor) were determined. Among the communities serviced by the chosen PHCs/CHCs, three villages-one close to one and two farther-were ultimately chosen, and they selected five non-patient homes from each of those villages. 62 PHCs, 31 CHCs, 224 patient households, 155 non-patient households, and 16 sample districts across eight states were chosen for the study. They also solicited the opinions of informed people in each selected village to prepare qualitative notes on the operation of healthcare institutions. Coverage of the Population & Location of CHCsIn 1996, a sub-center served 4737 people, a PHC served 28768, and a CHC served 2.6 lakh people across India. Thus, although there are variances between states and districts, on the whole, the population coverage of sub-centers and PHCs is substantially within the criteria established. However, in the case of CHCs, the population coverage is more than double the maximum (1.2 lakh) allowed by the standard. 
The population coverage of a CHC in the eight states under consideration ranged from a minimum of 1.3 lakh persons in Rajasthan to a maximum of 5.1 lakh in Bihar. Likewise, the typical number of Between 6 PHCs in Maharashtra and roughly 20 in Tamil Nadu are covered by a CHC. The Goals of CHC's of Regular Medical Clinics.CHCs provide accessible, integrated, and inclusive services for their intended population of people with some other group programs. Only community members are involved in program formulation and effective management at public health centers, which are accountable to the populations they represent. Community Healthcare Facilities by NationsCanada In Ontario, Community Health Centers (CHCs) have been around for over 40 years. In 1926, Mount Carmel Clinic became the first recognized CHC in Canada. An interdisciplinary team of healthcare professionals using electronic health records makes up the majority of CHCs. Local community services centers in Quebec, also referred to by its French abbreviation, CLSC, provide standard medical and social services, such as general practitioner appointments and walk-in consultations. Indonesia Puskesmas, a community health center or Pusat Kesehatan Masyarakat in Indonesian, are government-mandated community health centers. They administer healthcare for the populace at the sub-district level under the direction of the Indonesian Ministry of Health. The idea was developed by Johannes Leimena, the third Minister of Health of Indonesia, and was carried out by G. A. Siwabessy during the New Order era. The Indonesian health system also included community and preventive health programs. The Indonesian Health council says 9718 Puskesmas living in the nation. Portugal The health centre, or centre de sade in Portuguese, served as the regional public health authority and the virtual community primary healthcare unit of Portugal's National Health Service. Each health centre typically served a Portuguese municipality. However, places, where there is More than one of these centers can help a population of over 15 000 people. General practitioners, public health doctors, nurses, social workers, and office employees worked in health facilities. The almost 300 health facilities in 2008 were grouped into roughly 70 health centre groups, or ACES (arguments de Centros de sade). These are now the fundamental primary healthcare providers of the Portuguese National Health Service, and each ACES comprises several families and individualized healthcare units. The ACES provides essential medical emergency services, public health, community health, speciality units, and family health care services. Some ACES were combined with hospital units to form experimental local health units, also known as ALS. The ULS is meant to provide both treatments through the same health unit, making coordinating primary and secondary healthcare more accessible. British Empire In the United Kingdom, an NHS health facility (Murphy Philipps Architects). To create a report on "schemes necessary for the systematized supply of such forms of medical and related services as should... be available for the residents of a specific area," Christopher Addison hired Bertrand Dawson. Although no subsequent study was published, the Interim Report on the Future Provision of Medical and Allied Services was created in 1920. The report included extensive architectural renderings of various types of centres and detailed designs for a network of Primary and Secondary Health Centers. The phrase "health centre" was frequently used by 1939 to describe brand-new structures containing local health authority functions. Primary care received much less focus and funding than hospital services, and the local government's responsibility was the construction of health facilities from 1948 until 1974. In October 1952, a renowned facility was inaugurated at Woodberry Down. It contained space for six general practitioners, two dentists, a pharmacy, and two nurses. About £163,000 was spent on it. This also covered the price of daycare and a counselling centre for kids. Critics viewed this as expensive and used it as a justification for not constructing more. The new town corporation established four facilities in Harlow, making it the only municipality in Britain where doctors only practice outside health centres. In a sea of General Practitioners who were generally unconcerned with their success, the few constructed centres "functioned as isolated islands." Later, there were requests to create a network of clinics that would encompass not just general practitioners but also dentists and diagnostic services. There were 59 in Scotland, 29 in Wales, and 566 in England as of 1974. Following the National Health Service Reorganisation Act of 1973, Area Health Authorities took over responsibility for marketing health centres, and there were new calls for creating more Health Centers. When a patient's doctor is unavailable or when an emergency arises, it was suggested that these facilities might arrange for alternate medical care for them. When Lord Darzi served as a minister in 2008, he established a network of Polyclinics in England. These clinics shared specific characteristics with initial health centre concepts, but they also encountered a lot of GP opposition. The United States A community health centre is a nonprofit, patient-focused healthcare organization that offers access to first-rate, reasonably priced general and preventive healthcare and dental and mental health services. The specific goal of community health centres is to provide access for underserved, underinsured, and uninsured individuals. Community Health Centers (CHCs) are local clinics that primarily provide primary medical treatment to those who live in Medically Underserved Areas (MUAs), including uninsured, underinsured, low-income, or don't have easy access to it. Some health clinics have upgraded with new technology and computerized medical records, funding primarily from the federal and municipal governments. The Health Resources and Services Administration (HRSA) has identified certain places or groups as medically underserved because they lack primary care physicians, have high newborn mortality rates, high poverty levels, or have a significant senior population. HRSA has identified areas with a deficit of primary care, dental, or mental health professionals as health professional shortage areas (HPSAs), which might be geographical (a county or service region), demographic (low-income population), or institutional (comprehensive health centre, federally qualified health centre or another public facility). 2. Community Health CouncilStatutory ProvisionsAccording to the Community Health Councils (Access to Information) Act of 1988, community health councils were required to hold public meetings. They have a right to be consulted over the establishment of neighborhood pharmacies. Local governments appointed half of the members, local nonprofit groups appointed a third, and the Regional Health Authority, which provided funding for personnel and expenses, appointed a sixth. They have the right to be consulted before any changes are made to the health service or before any recommendations are made. There were numerous legal disputes about what constituted a substantial modification. Additionally, CHCs played a significant role in assisting those who complained about NHS services. 3. Community Health Clubs in AfricaCommunity health clubs (CHCs), also called community hygiene clubs, are nonprofit, neighbourhood-based organizations to promote hygiene and enhance public health in Africa. CHCs are created in each village. Africa AHEAD, a Zimbabwean NGO, originated and popularised the idea. 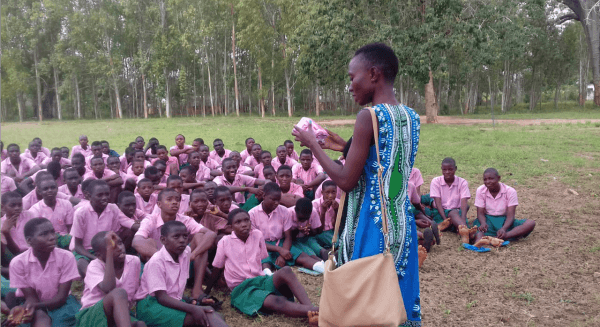
HistoryIn Kenya, where Juliet Waterkeyn created graphics for training materials used by the Kenya Water for Health Organization, the concept of CHCs first appeared (KWAHO). She studied rural Kenyan people's customs and way of life and asserted that the reason for the slow growth of communities was a lack of ownership. To bring people together and have a community discussion about hygiene for the sake of children's health, They developed the CHC concept. They go through a week of training, providing the necessary supplies and showing how to use them. Classic and Lite CHCs are the two categories. An elected six-member committee, a chairperson, a secretary, and a facilitator who is a Community Health Worker (CHW) are all included in the average membership of 75 for CHCs. The facilitator is in charge of facilitating discussion groups and inspiring the club members to practice better hygiene. Lite CHCs undergo a three-month training period and undertake eight conversation sessions in which they only cover WASH-related issues. Members are given homework after each session and urged to before the next session, finish it. When a person joins the club, they receive a membership card, and it is the CHW's responsibility to check off each member's attendance at conversation sessions. Promotion of HealthEach week, members gather for a two-hour meeting. Members are encouraged to participate in conversations and debates about issues promoting health and hygiene using cards during these sessions. Different interactive activities are conducted to amuse and motivate participants to participate in the decision-making process towards enhancing everyday hygiene practices. Each week, members are urged to make minor adjustments in their own houses. Rarely do these advised methods necessitate spending money and are solely habit-changing.
Next TopicFull Form
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










