Colonoscopy AlternativesA colonoscopy is a procedure doctors use to examine the large intestine for abnormalities, most commonly when screening for colorectal cancer. A healthcare professional inserts a long tube called a colonoscope into the rectum and along the length of the colon during the procedure. 
This tool generates images that aid in identifying colon polyps and can also remove them via a small wire loop attached to the tube. Colonoscopy can be expensive, have unpleasant side effects, and necessitate extensive preparation and sedation. Colonoscopy was once thought to be the most effective colorectal cancer screening tool. Recent guidelines acknowledge that other methods, depending on a person's level of risk and other factors, can be just as effective. 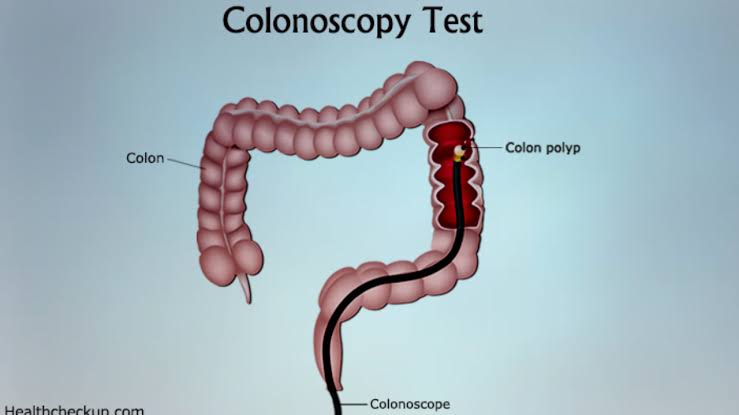
The sections that follow go over seven different colorectal cancer screening methods. 1. Faecal Immunochemical TestingStool samples are analysed in faecal immunochemical testing (FIT). FIT is a popular screening method in many parts of the world, and the Food and Drug Administration (FDA) has approved its use by Trusted Source. FIT employs antibodies to detect traces of blood in the sample, indicating bleeding in the gastrointestinal (GI) tract. Before providing a stool sample, a person should inform a doctor if they have haemorrhoids, anal fissures, or are menstruating to help avoid inaccurate results. The person collects a stool sample at home and brings it to the doctor for this test. FIT is covered by most insurance companies and is inexpensive. FIT is typically repeated every 1-2 years, depending on the doctor's recommendations. If the FIT results indicate GI bleeding, the doctor may recommend a colonoscopy for further evaluation. 2. Faecal Occult Blood TestA faecal occult blood test, an alternative to FIT, involves analysing a stool sample. The ACP recommends high-sensitivity guaiac-based faecal occult blood tests (gFOBT). A person should have a gFOBT screening every two years for it to be effective. If the results of the test indicate that there may be an abnormality in the GI tract, your doctor may advise you to have a colonoscopy. 3. Stool DNAThis test looks for blood and specific DNA in a stool sample to see if there is colon cancer. A stool DNA test, in addition to FIT, may be used by a doctor. If the test reveals any abnormalities, the patient may need to have a colonoscopy. 4. SigmoidoscopyA sigmoidoscopy is similar to a colonoscopy except that it examines a smaller portion of the large intestine. The sigmoidoscopy procedure is invasive and requires preparation, such as fasting and taking pills to induce diarrhoea or having an enema to clear the colon. This method is less risky than a colonoscopy and is often less expensive. However, it does not evaluate the entire colon. A doctor can explain the advantages and disadvantages of colonoscopy and sigmoidoscopy to each patient. 5. CT ColonographyThe procedure of CT colonography entails taking detailed images of the colon. Sedation is not required for the procedure. However, as with a colonoscopy, a person must first use medications or an enema to clear the colon. A healthcare professional will inflate the colon with air during the procedure to provide a better view. A colonoscopy is required if the test reveals an abnormality. 6. Double Contrast Barium EnemaA double contrast barium enema is an X-ray procedure that allows a doctor to examine the colon. The barium aids in the creation of clear images of the colon. This method is rarely used by doctors because, unlike colonoscopy, it does not detect small polyps and tumours. It is, however, an option for people who are at risk of colonoscopy complications. 7. A Single Speciemen gFOBTSome doctors collect a single stool sample during a routine rectal examination and analyse it with gFOBT. However, research has not shown that this is an effective method of screening for colorectal cancer. Adults with an average risk of colorectal cancer should have screenings between the ages of 50 and 75, according to American College of Physicians (ACP) guidelines published in 2019. According to the guidelines, a person and a doctor should decide on the method of screening based on a discussion of the following:
Colorectal cancer can be detected using faecal testing, colonoscopy, and sigmoidoscopy, according to researchers. The best screening method for each individual depends on their risk factors and preferences. Annual FIT or regular sigmoidoscopy or colonoscopy, according to BMJ guidelines, has reduced the incidence of cancer. However, when compared to sigmoidoscopy and colonoscopy, the incidence reduction of FIT is small. Colonoscopies and sigmoidoscopies can aid in the prevention of colorectal cancer by detecting adenomas, which appear before a tumour forms. Stool sample tests, on the other hand, cannot prevent colorectal cancer. They can only help a doctor detect it once it is present. The ACP recommends the following options for adults aged 50-75 years with an average risk of colorectal cancer:
Next TopicDiscord Alternatives
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










