What is the full form of DVT
DVT: Deep Vein Thrombosis
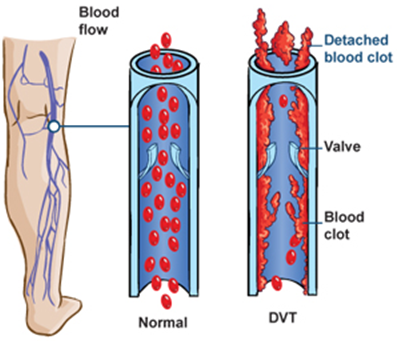
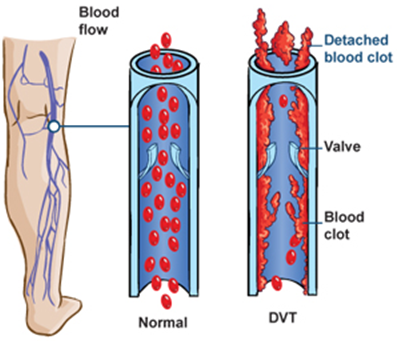
DVT stands for Deep Vein Thrombosis. It refers to a blood clot that forms in a vein located deep inside your body, usually in the lower leg or thigh. However, it can occur in other parts of the body. Such clots are usually formed when a vein is damaged, or blood flows slowly or stops flowing in a vein. It usually affects people of age 50 or more. DVT is a serious medical condition, so you should consult your doctor immediately if you are experiencing symptoms of this medical condition.
Causes
The following factors can increase the risk of developing thrombosis:
- Damaged vein due to an injury such as a bone fracture.
- Obesity tends to put more pressure on the veins located in the legs or pelvis
- Family history of DVT
- Use of birth control pills
- Undergoing hormone replacement therapy
- Prolonged bed rest, such as during hospitalization
- Inflammatory bowel disease
- Heavy smoking
- Sitting for a longer duration, such as when driving or flying for longer durations, or the job of a watchman.
Common Symptoms:
- Swelling in your leg, foot, or ankle, usually on one side
- Cramping pain in the affected area of the leg
- Severe pain in the foot or ankle
- Redness over the affected area
- Warm sensation over the affected area
Complications:
- Pulmonary embolism: It occurs when the blood clot breaks off, and its pieces start traveling in the bloodstream, and one of the pieces blocks a blood vessel that carries blood to the lung.
- Post-thrombotic syndrome: It is chronic venous insufficiency following DVT. It occurs when the DVT damages the valves of the vein, and the blood, instead of moving upwards, starts accumulating in your lower leg. It causes long-term pain, swelling, and ulcers in some cases.
- Limb ischemia: It occurs in severe cases of DVT. In this complication, due to the blood clot, the pressure in the vein becomes very high, which tends to block blood in the arteries and thus restricts oxygen supply to the affected area. It is usually painful and may cause skin ulcers and gangrene.
When to visit a doctor
Whenever you get DVT symptoms, get in touch with your doctor.
If you encounter any of the potentially fatal symptoms of a pulmonary embolism (PE) or a deep vein thrombosis complication, seek emergency medical assistance.
The following signs and symptoms of a pulmonary embolism include:
- Abrupt lack of breath
- Chest discomfort or pain that worsens with heavy breaths or coughing
- Feeling faint or disoriented
- Fainting
- Fast heartbeat
- Quickly breathing
- Exhaling blood
Risk elements
Many variables might raise the possibility of deep vein thrombosis (DVT). The risk of acquiring DVT increases as your risk factors do. DVT risk factors include:
- Age: DVT risk goes up after 60 years of age. Yet, DVT may happen at any age.
- Absence of motion: When the legs remain stationary for a lengthy period of time, the calf muscles do not contract (contract). Blood flow is aided by muscle contractions. DVT risk is increased by prolonged sitting, such as when driving or flying. The same is true for prolonged bed rest, which may be brought on by a protracted hospital stay or a physical condition like paralysis.
- Injury or operation: Surgery or vein damage may raise the risk of blood clots.
- Pregnancy: During pregnancy, the stress in the veins of the legs and pelvis increases. The possibility of a blood clot from pregnancy may persist for as long as six weeks after the baby is born.
- Hormone replacement treatment or oral contraceptives for contraception.
- Being fat or overweight: When a person is overweight, the pressure in the veins of the legs and pelvis increases.
- Smoking: Smoking affects blood flow and coagulation, which raises the chance of DVT.
- Cancer: Certain malignancies increase the blood's clotting-causing chemicals. The risk of blood clots can increase with several cancer treatments.
- A heart attack: DVT and pulmonary embolism risk factors for heart failure are higher. Those with heart failure have impaired heart and lung function, making even a tiny pulmonary embolism more obvious.
- Colon inflammation: Both ulcerative colitis and Crohn's disease increase the risk of DVT.
- A PE or DVT history, either personal or familial: If each of these conditions has been experienced by you or a family member, you may be more susceptible to developing DVT.s
- Genetics: Blood clots more readily in some persons due to Genetic alterations. Leiden's factor V is one illustration. This inherited disorder changes one of the blood's clotting factors. Blood clots may not be brought on by an inherited condition on its own unless additional risk factors are present.
Sometimes a blood clot in a vein develops without any clear risk factors. An unprovoked VTE is what it is known as.
Diagnosis:
On the basis of symptoms, if your doctor thinks that you might have a DVT, he or she may perform the following tests to diagnose DVT.
- D-Dimer: It is a blood test that is performed to detect the pieces of the blood clot that travel in the bloodstream after the breakdown of the blood clot. A large number of pieces indicate the presence of blood clots in the vein.
- Doppler ultrasound: In this test, sound waves are used to monitor the blood as it flows through the blood vessels. It is suitable for identifying large blood clots above the knee.
- Venogram: In this test, a special dye is injected into the veins in the foot, and then an X-ray of the veins is taken to see if there is a clot in a vein. It is an ideal test to detect blood clots below the knee.
Prevention:
- Avoid sitting or standing still for long durations
- Make positive lifestyle changes
- Regular exercise
- Avoid heavy smoking
- Maintain ideal body weight
- Maintain a healthy diet
- Increase fluid intake
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now










