What is the full form of FSHFSH: Follicle Stimulating HormoneFSH stands for Follicle Stimulating Hormone. It is a hormone in the human body, and the hormone is nothing but a protein that is created by the pituitary glands. The Follicle Stimulating Hormone (FSH) makes a condition for the growth of follicles of the ovaries and maintains regularity in the menstrual cycle. 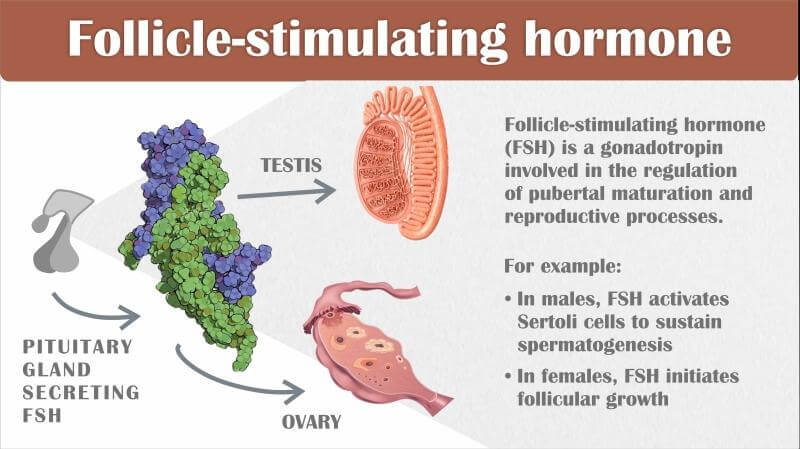
What is FSH or Follicle Stimulating Hormone?The Follicle Stimulating Hormone (FSH) has a significant role in the formation and growth of eggs in women, along with maintaining menstrual cycles. They are not only present in females but also in males. In men, FSH, or follicle-stimulating hormone, plays an important role in the production of sperm. Hence, follicle-stimulating hormone (FSH) plays a vital role in women's and men's reproduction organs. The Follicle Stimulating Hormone (FSH) is created in the brain, specifically in the pituitary gland. However, the level of Follicle Stimulating Hormone (FSH) present in the body can be measured by a blood test. An abnormal level of this hormone displays issues in fertility. What is the work of FSH or Follicle Stimulating Hormones?The Follicle Stimulating Hormone (FSH) is an essential hormone for reproduction as well as sexual health. The following are the functions of the Follicle Stimulating Hormone (FSH):
What is the Follicle Stimulating Hormone (FSH) test?As we know, the follicles are tiny sacs in the ovary which contain eggs, which is also necessary for the maintenance of sexual health and reproduction. The FSH test is a blood test that helps know the hormone's status in the human body. It is also used to solve the issues with ovulation, if any. If a woman is not ovulating, then there is a high chance that the FSH levels in such women are high. Women undergoing menopause also have higher FSH levels. Also, it is to be noted that even if the woman is taking fertility drugs, the level of the hormone FSH is high. The count of the FSH can be different throughout a menstrual cycle. In the early follicular phase, when the ovaries begin to grow new eggs, the hormone level is generally high. However, during the late luteal phase after ovulation, they are comparatively lower in the count. Hence, the FSH test can determine whether ovulation in women is taking place. On the third, fifth, and seventh days of the menstrual cycle, the FSH levels are usually monitored, and the count on the seventh day is typically high. It is also said that a patient can undergo an FSH level test while undergoing the in - vitro fertilization (IVF) treatment. The following are the conditions when anyone should go to test their FSH level:
What is the normal level of FSH or Follicle Stimulating Hormone?The range of the Follicle Stimulating Hormone (FSH) varies depending on the status of puberty in the body. They are as follows:
What is the outcome of an abnormal Follicle Stimulating Hormone (FSH) count?The following are the repercussion of having high Follicle Stimulating Hormone (FSH) levels:
The following are the repercussion of having low Follicle Stimulating Hormone (FSH) levels:
The Female Reproductive System and FSHa. Role in the development of ovarian follicles:FSH is essential for ovarian follicle formation and expansion in the female reproductive system. Small, fluid-filled sacs called ovarian follicles are found inside the ovaries and house immature eggs or oocytes. Several follicles start to form under the influence of FSH throughout each menstrual cycle. The granulosa cells of the ovarian follicles are affected by FSH, which encourages their development and proliferation. In preparation for a prospective pregnancy, the endometrium (the uterus lining) continues to expand as a result of the follicles' production of estrogen as they develop. b. Production of Estrogen and FSH:FSH encourages the granulosa cells in the developing ovarian follicles to change androgens (male hormones) into estrogens (female hormones), especially estradiol. The growth and maturity of the follicles depend on the presence of estrogens. The quantity of estrogen produced by the follicles rises as they develop and become more mature. The menstrual cycle is significantly regulated by estrogen. It encourages the endometrium's thickness, boosting its development and vascularity and laying the groundwork for possible embryo implantation. c. Ovulation and FSH:Ovulation, or the release of a mature egg from the ovary, is a process that is aided by FSH. One dominant follicle forms and becomes the main site of FSH activity as the follicles continue to grow. The dominant follicle's increased estrogen levels have a positive feedback effect on the pituitary and brain. GnRH, FSH, and LH production increase as a result. The release of the mature egg from the dominant follicle, or ovulation, is one of the last phases of follicular maturation that are triggered by the LH surge. The release of the egg, which allows for the possibility of sperm fertilization, usually takes place around the halfway point of the menstrual cycle. If fertilization takes place, the fertilized egg implants into the endometrium that has been prepared, beginning the pregnancy. d. Ageing and FSH:The levels of FSH and other reproductive hormones decrease significantly throughout menopause, which signifies the end of a woman's fertile years. The reduced ovarian function causes a drop in follicle quantity and quality, which lowers estrogen output. The hypothalamus and pituitary gland notice the drop in estrogen levels and try to make up for it by secreting more FSH. As a result, blood tests may be performed to quantify higher FSH levels in menopausal women, which are used to evaluate ovarian reserve and reproductive function. Hot flashes, mood swings, and vaginal dryness are menopausal symptoms that can be linked to hormonal imbalances, particularly elevated FSH levels, during this transitional stage. In conclusion, by boosting the synthesis of estrogen, enabling ovulation, and encouraging the growth and development of ovarian follicles, FSH plays a critical function in the female reproductive system. The normal operation of the menstrual cycle and fertility depends on it. The Male Reproductive System and FSHa. FSH and spermatogenesis:FSH is a critical component in the process of spermatogenesis, which is the development and maturation of sperm cells within the testes in the male reproductive system. Seminiferous tubules are microscopic organs where spermatogenesis takes place. The Sertoli cells, which are found inside the seminiferous tubules, are affected by FSH. These cells help sperm cell development structurally and nutrient-wise. The production of proteins and other elements required for the development of sperm cells is stimulated by FSH in Sertoli cells. The development of spermatogenesis depends on the presence of FSH. It encourages spermatogonia (sperm precursor cells) to divide and differentiate into spermatocytes, which produce mature sperm cells. b. FSH and the production of testosterone:The generation of testosterone in the male reproductive system is likewise controlled by FSH. The main male sex hormone, testosterone, is in charge of many aspects of male development and reproductive health. Leydig cells in the testes create testosterone when luteinizing hormone (LH), a different hormone, is present. FSH does, however, indirectly support the synthesis of testosterone by preserving the ideal conditions for Leydig cell activity. The Sertoli cells, which support and feed the Leydig cells, are affected by FSH. Under the effect of FSH, Sertoli cells release a number of substances, including androgen-binding protein (ABP). ABP aids in the concentration of testosterone within the seminiferous tubules, fostering spermatogenesis and boosting sperm cell maturation. c. Insomnia and FSH:Hypogonadism is a disorder in which the testicles don't generate enough testosterone, which can cause a number of symptoms and reproductive issues. FSH levels are frequently increased in cases of primary hypogonadism, which is brought on by testicular dysfunction. As a coping mechanism, hypogonadism results in elevated FSH levels. The brain and pituitary gland detect low testosterone levels and boost the release of gonadotropins, particularly FSH, in an effort to enhance testicular activity when the testes are unable to generate enough testosterone. In order to identify and evaluate the root causes of male infertility and hypogonadism, FSH levels can be measured. While normal or low FSH levels may point to a hypothalamus or pituitary problem, high FSH levels, together with low testosterone levels, may indicate primary testicular failure. In conclusion, by stimulating the synthesis of testosterone and fostering spermatogenesis, FSH plays a crucial function in the male reproductive system. It helps maintain ideal circumstances for Leydig cell activity and operates on Sertoli cells to speed up sperm cell development. FSH level dysregulation may be a sign of male infertility and malfunction of the testicles. FSH Clinical Importancea. Testing for FSH and its InterpretationFSH testing is frequently done on both males and females to evaluate how well their reproductive systems are functioning. FSH levels are measured by blood testing, and the outcomes are helpful in both detecting and treating a variety of reproductive diseases. FSH levels in females are routinely assessed at particular points during the menstrual cycle. Elevated FSH levels may be a sign of lower ovarian reserve, which is characterized by fewer follicles and decreased reproductive potential in the ovaries. Low FSH levels may indicate hypothalamic or pituitary malfunction, which can cause amenorrhea (the lack of menstruation) or irregular menstruation. FSH levels in males are frequently assessed with hormones like testosterone and LH. Low testosterone levels and elevated FSH levels may be signs of primary testicular failure. On the other hand, low FSH levels in the presence of low testosterone may point to a pituitary or hypothalamic issue. b. Levels of FSH During Pregnancy:FSH levels normally remain low during pregnancy. This is so that pregnancy can occur, which entails blocking the formation of follicles and suppressing the menstrual cycle. The synthesis of the hormones required to maintain pregnancy is taken up by the placenta, and FSH is reduced to stop the growth of new follicles. It is not common practice to check FSH levels during pregnancy since it is difficult to interpret them at this time. FSH levels, however, may be abnormal during pregnancy if certain diseases, such as PCOS or ovarian cysts, are present. c. FSH in the Assessment of Infertility:Both male and female infertility can be assessed with the FSH test. FSH levels in females can be used to evaluate ovarian reserve and predict how well in vitro fertilization (IVF) therapies could work. Low FSH levels may indicate insufficient ovarian stimulation, whereas elevated FSH levels may indicate a lower reproductive potential. FSH levels and other hormone evaluations can help men diagnose infertility and determine its underlying causes. While low FSH levels may point to a hypothalamic or pituitary problem, elevated FSH levels may indicate intrinsic testicular failure. FSH testing is frequently paired with other hormone tests, imaging scans, and other tests to offer a thorough review of reproductive function and to help choose the best course of therapy. In conclusion, FSH testing plays a crucial role in identifying infertility in both males and females and evaluating reproductive function. It aids in the assessment of ovarian reserve, the detection of testicular dysfunction, and the formulation of effective treatment plans. FSH level interpretation is crucial and frequently done in combination with other hormone testing and clinical assessments. Conditions Related to FSH Dysregulationa. PCOS (polycystic ovary syndrome):A common hormonal condition in women known as polycystic ovary syndrome (PCOS) is characterized by an abundance of tiny ovarian cysts, irregular menstruation periods, and high levels of androgen (male hormone). Some PCOS patients have FSH dysregulation. The typical hormonal balance and feedback mechanisms are disrupted in PCOS due to the high amounts of androgens. A relative rise in LH levels results from the decreased FSH production caused by elevated testosterone levels. The hormonal imbalance contributes to irregular menstrual cycles and the development of ovarian cysts by interfering with normal follicular development and ovulation. b. Ovarian Insufficiency Premature (POI):When the ovaries stop functioning normally before the age of 40, the condition known as premature ovarian insufficiency (POI), commonly referred to as early ovarian failure, occurs. Ovarian dysfunction in women with POI leads to decreased estrogen levels, irregular menstruation cycles, and infertility. Due to a decreased ovarian reserve, there may occasionally be a rise in FSH levels with POI. The brain and pituitary gland increase FSH production in an effort to stimulate the ovaries in response to the decreasing quantity and quality of follicles. POI may be indicated by elevated FSH levels in the absence of healthy ovarian function. c. Hypogonadism in MenMale hypogonadism is a disorder where the testes don't generate enough testosterone, which can cause a number of symptoms like decreased libido, erectile dysfunction, exhaustion, and infertility. There can be FSH dysregulation in some forms of male hypogonadism. Primary testicular failure, or primary hypogonadism, is a condition in which the testes are unable to generate enough testosterone. FSH levels are frequently increased as a compensatory reaction in primary hypogonadism. The decreased testosterone synthesis and the hypothalamus-pituitary axis's efforts to boost testicular activity are reflected in the higher FSH levels. d. FSH's Function in Assisted Reproductive Techniques (ART):In vitro fertilization, (IVF) and other assisted reproductive methods depend heavily on FSH. In IVF, numerous follicles are encouraged to grow and mature through controlled ovarian stimulation before being removed for fertilization. Exogenous FSH is given to the patient in the form of fertility drugs to activate the ovaries and encourage follicular development. A regulated and balanced response to FSH is desired in order to promote the growth of the ideal number of mature follicles that are ready for fertilization. The effectiveness of ART techniques can be impacted by FSH dysregulation or a poor response to exogenous FSH stimulation. To get the best results in these situations, careful monitoring of FSH levels and customized changes of fertility medicines are required. In conclusion, FSH dysregulation is linked to a number of reproductive diseases. Primary testicular failure and some forms of male hypogonadism can cause increased FSH levels in men, although excessive FSH levels can be seen in disorders including PCOS and POI. For the diagnosis and treatment of these illnesses as well as for enhancing the success of assisted reproductive technologies, it is essential to comprehend FSH dysregulation. Applications in Medicine and Future Prospectsa. FSH Therapeutic Applications
b. Future Research and Perspectives
In conclusion, FSH has shown therapeutic benefits in the treatment of hypogonadism, ovulation induction, and assisted reproductive technologies. Personalized medicine, FSH receptor modification, new FSH preparations, fertility preservation, and deciphering FSH control are the main areas of current research and future possibilities. These developments have the potential to advance fertility therapies, improve patient outcomes, and deepen our knowledge of reproductive health. ConclusionFollicle Stimulating Hormone (FSH), in conclusion, is essential for both the male and female reproductive systems. It is necessary for the expansion and maturation of ovarian follicles, the synthesis of estrogen, and the start of ovulation in females. FSH encourages the synthesis of testosterone and sperm in males. Several reproductive illnesses, such as polycystic ovary syndrome (PCOS), premature ovarian insufficiency (POI), and male hypogonadism, are linked to the dysregulation of FSH levels. In addition to helping diagnose and treat these disorders, FSH testing is useful for evaluating both male and female reproductive potential. Important new information on ovarian reserve, ovarian function, and testicular function is provided. In order to maximize the effectiveness of therapy, FSH levels are monitored during assisted reproductive technologies (ART). FSH has medicinal uses in the treatment of hypogonadism, ovulation induction, and assisted reproductive technologies. Exogenous FSH is given as part of fertility treatments to promote follicular development, trigger ovulation, and treat hormonal abnormalities. Personalized medicine, FSH receptor modulation, new FSH preparations, fertility preservation, and further deciphering the nuanced control of FSH production are the main areas of the current study. Future advances in reproductive treatments, personalized strategies, and cutting-edge therapeutic techniques may be made thanks to these developments. They also help us understand reproductive health better and may inspire fresh approaches to treating reproductive problems. In conclusion, FSH is an important hormone that has a variety of roles in both the male and female reproductive systems. Dysregulation of it may have important effects on ovulation and reproductive health. FSH has the potential to significantly improve the diagnosis, management, and treatment of reproductive diseases via ongoing research and strides in therapeutic applications, thereby raising the quality of life for those looking to start children as well as single people and couples.
Next TopicFull Form
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










