What is the full form of LSCS
LSCS: Lower Segment Caesarean Section
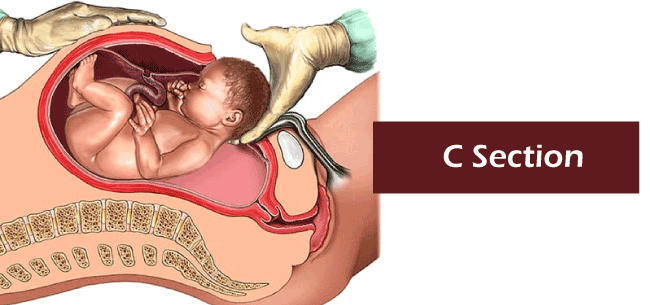
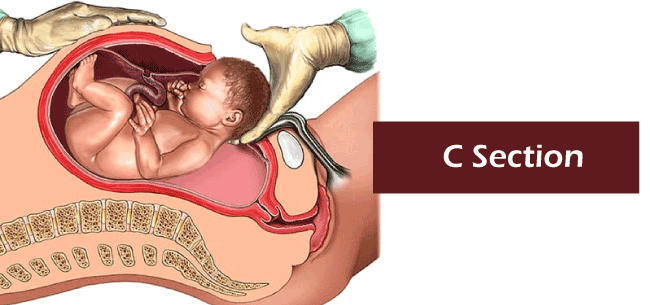
LSCS stands for lower segment caesarean section. The most common kind of Caesarean section performed is called a Lower Segment Caesarean Section (LSCS). The lower uterine segment is usually cut transversely above the point where the urine bladder attaches to the uterus to deliver the baby.
History And Origin
German gynecologist Hermann Johannes Pfannenstiel invented the method. The procedure is commonly referred to as the Kerr incision, or the Pfannenstiel-Kerr cut in English-speaking nations, since Dr Monroe Kerr performed the process for the first time in Great Britain in 1911 and popularized it there. In 1920, Kerr reported that the previous technique harmed vascularized parts of the uterus more than a C-section. Vascularized parts of the uterus include the endometrium, myometrium and perimetrium. He claimed it was preferable to a longitudinal uterine cut in terms of scar rupture and artery damage.
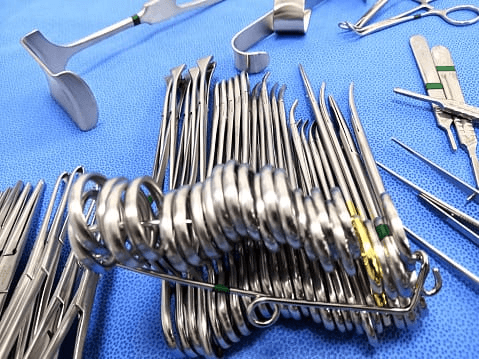
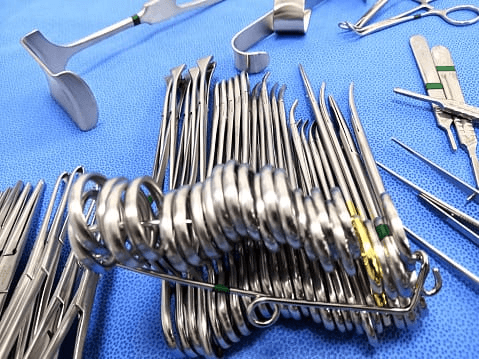
Forceps can be used to reduce bleeding since most bleeding occurs from the direction of the cut. Forceps from the Green Armytage line are made specifically for this use.
Even though a sharp scalpel is used to cut, caution must be exercised to avoid harming the foetus, mainly if the membranes are burst or in situations like abruption. With the use of scissors or rough dissection with the hands, the cut can be stretched on either side. The gynaecologist should insert a finger below the uterus before using the scissors to avoid unwanted harm to the foetus. Blood loss during surgery can be reduced if rough dissection is used.
When the Pfannenstiel incision cannot be performed (for example, when the baby is young), the uterus may be removed using a J-shaped cleavage, a T-shaped surgery, a Kronig incision (low vertical incision), or a classical incision (midline). An incision is made in the abdominal and uterine walls during an operation to deliver foetus after completing the 28th week. The c-Section technique consistently improves surgical safety and blood transfusions.
Factors For Rising Cesarean Section Rate
- Detection of foetuses at risk
- Identifying moms (pn) who are at risk
- Expanding the availability of repeat cs in the circumstances involving prior cesarean deliveries, increasing rates of labour induction, and inability to induct
- The decline in manipulative natural delivery (rotational forceps) and operational cesarean section (mid forceps, suction)
- Decreased rate of vaginal cesarean birth and related health problems
- Neither the mothers nor the gynecologists are willing to accept the risk of unusual childbirth.
- Greater detection of pregnancy complications and expanded usage of electronic foetal surveillance.
- There is a great fear of legal action in the profession of obstetrics.
Various Indications Regarding The Childbirth Through C-Section
Absolute indication: vaginal birth is impossible;
Relative indication: vaginal birth is an option, but there are risks for both the mother and the infant
Signs Of Absolute Indications For A C-Section
- placenta in the centre of Previa
- a contracted pelvis or an abnormal cephalopelvic ratio (absolute)
- Pelvic mass obstructing motion (cervical or broad ligament fibroid)
- advanced cervical cancer
- the obstacle to vaginal flow (atresia, stenosis)
Common Symptoms Of Absolute Indications
Primigravidae
- neglected sign
- neglected foetal distress (non-reassuring Fetal FHR)
- Cephalo Pelvic Disproportion (CPD)
- Dystocia (dysfunctional Labor); and
- malposition and malpresentation (occiput posterior, breech).
Pre-Caesarean birth, antepartum haemorrhage (placenta praevia; placental abruption), and malpresentation are all symptoms of multigravidae (breech, transverse lie).
Relative Indicators
Although giving delivery naturally may be possible, there are severe risks for the mother and/or the baby.
Other factors include;
- misaligned cephalopelvic region (relative)
- before surgical delivery, the major
- consistent hint led to CS (contracted pelvis).
- The two CS from previously.
- The properties of scar dehiscence.
- Formerly known as CS3.
- Uncomfortable FHR (fetal distress)
- A relatively big foetus (passenger), a limited pelvis (passage), or ineffective uterine contractions may all contribute to dystocia (Power)
- Placenta previa and abruptio placenta are two examples of antepartum bleeding.
- Breech, shoulder (transverse lying), and brow malpresentation
- Failure to advance in labour after an unsuccessful surgical induction of labour
- unfavourable obstetric history, including repeated foetal loss
- Pre-eclampsia with severe complications and uncontrollable fits despite anti-seizure treatment are two examples of hypertensive diseases
Uncontrolled diabetes, heart disease (coarctation of the aorta, Marfan's syndrome), mechanical blockage brought on by benign or malignant pelvic tumours (carcinoma cervix), or as a result of vesicovaginal fistula repair are examples of medical-gynaecological problems.

Timing
- Elective: Completed at a scheduled time
Advantages
- There is no risk associated with labour or delivery.
- There are no pelvic floor issues.
Hazards
- Preterm birth and hysterectomy
- prolong hospital stays and recuperation times.
Election Timing
- Maturity is unavoidable
- Approximately one week before the anticipated date of confinement (EDD)
Maturity Is A Mystery
- first or second-trimester ultrasound evaluation
- To verify foetal maturity, amniocentesis is performed for the L:S ratio.
- Otherwise, CS is stopped while waiting for the commencement of spontaneous labour.
- Emergency: Done as a result of an immediate obstetric emergency. (A half-hour stretch of duration.)
Category 1
- When the woman's or the fetus's life is immediately in danger.
- The delivery interval for decisions should be 30 minutes.
Category 2
- When a maternal or foetal condition that is not urgently life-threatening compromises those conditions.
- CS must be completed within 75 minutes of choice being made.
Category 3
There is no foetal or maternal impairment, but an early delivery is necessary.
Category 4
The timing of the delivery is chosen to accommodate the mother, her loved ones, and the medical personnel.
Preparation for Surgery
- Written informed consent is acquired for the surgery, anaesthesia, and blood transfusion.
- With soap and nonorganic iodide lotion, the abdomen is cleansed.
- One may trim one's hair.
- No premeditative sedatives should be administered.
- Oral administration of a non-particulate antacid (0.3 molar sodium citrate, 30 ml)
- The H2 blocker ranitidine is administered orally at 150 mg the night before an elective procedure and 50 mg IM or IV the following morning.
- Emptying the stomach is advised. -Stomach tube (emergency procedure).
- Metoclopramide (10 mg IV) was administered to reduce stomach contents and improve lower oesophagal sphincter tone.
- A Foley catheter left during the perioperative phase should be used to empty the bladder.
- At this point, FHS has to be tested once more.
- One should make a neonatologist available.
- Crossmatch savagery
- Before performing the skin incision, preventative antibiotics should be administered intravenously.
- 5% dextrose and ringer solution are administered using an IV cannula.
- cross-sectional abdominal incision.
Benefits
- Postoperative comfort is increased.
- Immediate postoperative recovery allows for better palpation of the uterus fundus and reduces the risk of wound dehiscence and incisional hernia.
- cosmetic worth
Disadvantages
- It is not appropriate in a time-sensitive emergency since it takes a bit longer.
- Blood loss is slightly higher.
- Competence is necessary throughout the repetition part. Unfit for traditional operation
Other uterine incision styles include
- Lower vertical, which may be extended upward as necessary; classical incision (upper segment).
- The first transverse incision was extended vertically in a "J" shape; the mid-transverse incision was extended in an inverted "T" shape.
- A vertical uterine incision is made when the lower segment is underdeveloped, when the anterior placenta previa is fully grown, or when any myona is occupying the lower piece, a vertical uterine incision is made.
Delivery of the head
- Rupture of the membranes; sucking of the blood-mixed amniotic fluid; removal of the Doyen's retractor.
- To deliver the head, hook it with your fingertips.
- The palm serves as a fulcrum while the head is delivered through elevation and flexion. The helper should push on the fundus as the head is brought near the incision line.
- Delivered utilising Wrigley's; push up the head with sterile fingers inserted into the vagina.
Delivery of the Trunk
- If the trunk mucus from the nose, throat, and mouth are expelled, 20 units of intravenous oxytocin or 0.2 mg of methacine should be given after the shoulders are delivered.
- The remainder of the body is given gradually.
- The baby's head is angled downward for gravity drainage and put on a tray between the mother's legs. The infant is given to the paediatrician after the chord is severed between two clamps.
- The Doyen's retractor has been brought back.
- Intervals of less than 90 seconds between uterine incision and birth are ideal; intervals of more than 90 seconds are associated with poor Apgar scores.
- The placenta and membranes are removed.
- The placenta spontaneously separates.
- The placenta is retrieved by applying pressure to the chord (controlled cord traction).
- The membranes are delicately extracted, ideally intact, and even a tiny piece, if linked to the decidua, should be removed using dry gauze.
- The uterine cavity should be investigated. The uterine wound's suture
- The uterus is kept within the abdomen while the uterine incision is sutured; other people, on the other hand, prefer to eventuate the uterus first.
- To grasp the wound's edges, use green Armytage hemostatic clamps or Allis tissue forceps (four are required, one for each angle and margin).
- The uterine incision has three layers of sutures.
First Layer
- The first stitch is positioned and knotted on the opposite side of the uterine incision at the lateral angle.
- The needle is round-bodied, and the suture material is neither "0" chromic catgut nor vicryl.
- A continuous running suture ensures adequate tissue apposition by taking deeper muscles while excluding or including the decidua (extremely difficult to exclude).
- The stitch is eventually secured once the suture encompasses the near end of the angle.
Second Layer
- The adjacent fascia and superficial muscles are wrapped in a similar continuous suture, which is covered over the first layer of the suture.
- A continuous single layer may be used to seal the uterine muscles.
- stitching across the entire muscle and decidua. In light of the possibility of future scar rupture, it is debatable whether the wound should be closed in a single or double layer.
- The continuous inverting suture may be used to attach the peritoneal flaps (to prevent any raw surface).
- The peritoneum visceral and parietal should not be closed.
- The mops put inside are taken out, and the number is checked.
- Peritoneal toileting is performed, and the blood clots are carefully removed.
- The ovaries and tubes are inspected.
- Doyen removes his retractor.
- The abdomen is closed in layers once it is determined that the uterus is constricted correctly.
- A sterile vulval pad is applied after clearing the vagina of blood clots.
Complications During Surgery
a. Intraoperative Complications
- widening of the uterine incision on one or both sides.
- Uterine wall laceration near the lower uterine incision
- Bladder injury-this could occur during the subsequent surgery.
b. Ureteral harm
- Damage to the gastrointestinal tract
- Haemorrhage
- Morbidly adherent placenta
- Postoperative compliments are as follows:
c. FETAL
- latrogenic prematureness
- RDS development
- The infant might receive an unintentional scalpel wound.
d. Maternal and perinatal death
a. Mothers can suffer from
(1) Shock and bleeding
(2) Anaesthesia Risks
(3) disease and
(4) Thromboembolic disorders
b. Fetal
To deliver a breech baby through a tiny incision, the foetus suffers from
(1) asphyxia,
(2) RDS,
(3) premature birth,
(4) infection, and
(5) brain haemorrhage.
c. Special C-Section
The following are the most common conditions:
- Morbid adherent placenta.
- Atonic uterus and unmanaged postpartum haemorrhage.
- Large fibroid (in parous women).
- Severe lacerations.
- Extensively infected uterus.
- Ruptured uterus.
Peripartum Hysterectomy
Surgery to remove the uterus during a caesarean delivery or in the first few weeks after giving birth is known as a peripartum hysterectomy (even following vaginal delivery).
Post-Mortem Caesarean Section
Perimortem caesarean birth occurs when a woman has her baby during an operation while she is either about to pass away or has already passed away. When the foetus is alive, it is completed four to five minutes after cardiopulmonary resuscitation (CPR) begins.
Subtotal Hysterectomy
Subtotal hysterectomy is frequently performed as an unanticipated (emergency) treatment.
Subtotal hysterectomy advantages include:
- Reduced blood loss, less operating time, and a lower chance of harm to other organs (bladder, ureter).
- postoperative complications are reduced
- A C-section delivered without the uterus is used in situations of severe infection.
- Dissecting via the retail area allows for extraperitoneal access to the lower segment.
- This is hardly done due to the availability of powerful antimicrobial medicines.

Traditional C-Section
- Easy to carry out.
- Every abdominal incision is 15 cm (6 inches) long and paramedian ("in length, with one-third hanging over the umbilicus.
- A 12.5 cm (5 inch) longitudinal incision ("SLI") is performed beginning below the fundus and moving along the midline of the anterior wall of the uterus.
- The incision is deepened along its entire length until the membranes are exposed which are punctured.
- Approximately 40% of the time, the placenta is discovered.
- In such circumstances, fingers are inserted until the membranes are reached between the placenta and the uterine wall.
- Breech extraction is the most frequent delivery method for babies.
- After the infant is delivered, methergine 0.2 mg or five iu of intravenous oxytocin (slow) is given. The uterus has been affected.
- The placenta is retrieved by pulling on the cord or by hand.
What medical conditions call for a C-section?
Your doctor may decide to plan a caesarean birth before your due date. Or perhaps a crisis during childbirth makes it essential.
The most frequent medical justifications for a caesarean section are listed below.
Prolonged Labour
According to the Centers for Disease Control and Prevention Trusted Source, prolonged labour, commonly referred to as "failure to progress" or "stalled labour," accounts for close to one-third of caesarean sections. It occurs when a new mother spends at least 20 hours in labour. Or, for mothers who have already given birth, 14 hours or longer.
Slow cervical thinning, carrying multiples, and having babies too big to get through the birth canal can make labour last longer. To prevent difficulties, physicians may recommend a caesarean section in certain situations.
Abnormal Positioning
Babies should be placed headfirst close to the birth canal to have a healthy vaginal delivery.
&But infants occasionally rewrite the rules. They can breach with their feet or butt towards the canal or transverse, with their shoulder or side facing the channel.
In these circumstances, especially for mothers bearing several infants, a caesarean section may be the safest delivery method.
Fetal Distress
If your baby is not getting enough oxygen, your doctor may decide to deliver through an emergency caesarean.
Congenital Disabilities
Doctors may opt to perform a caesarean delivery on newborns who have specific birth disorders, such as excess cerebral fluid or congenital heart problems, to lessen delivery difficulties.
Repeat Cesarean
According to the American Pregnancy Association, almost 90% of women who have undergone a caesarean delivery may give birth naturally to their subsequent child. This is referred to as vaginal birth following caesarean (VBAC).
To determine if a VBAC or repeat caesarean is the best and safest option, expectant mothers should see their doctor.
Chronic Health Condition
A woman with a chronic illness like heart disease, high blood pressure, or gestational diabetes may give birth by caesarean section. If a mother has one of these disorders, vaginal delivery might be risky.
Doctors will advise a caesarean section if the pregnant mother has HIV, genital herpes, or any other illness that might be passed to the baby during vaginal birth.
Cord Prolapse
Cord prolapse occurs when the umbilical cord passes through the cervix before labour and delivery. This might reduce the baby's blood flow, endangering the baby's health. The rare yet dangerous condition of cord prolapse necessitates an urgent caesarean delivery.
Cephalopelvic Disproportion (CPD)
A CPD occurs when the baby's head or the mother's pelvis is too big for the birth canal, or the mother's pelvis is too tiny for vaginal delivery. In any case, the baby cannot enter through the vagina.
Placenta Issues
When a low-lying placenta partly or wholly covers the cervix, doctors will perform a caesarean (placenta previa). When the placenta separates from the uterine lining, and the infant begins to lose oxygen, a caesarean is also required (placenta abruption).
According to the American Pregnancy Association, one in every 200 pregnant women experiences placenta previa. Placental abruption affects about 1% of pregnant women.
Carrying Multiples
Having multiples during pregnancy carries a variety of dangers. It may result in protracted labour, which might disturb the mother. There might be one or more infants in an unusual posture. The most secure method of delivery is usually a caesarean.
Takeaway
Pregnant women should be ready if a caesarean delivery is required because pregnancy and childbirth can occasionally be unanticipated. Being a mother is a remarkable experience; therefore, it's best to be as ready as you can be for the unexpected.
Conclusion
Most caesarean sections are performed in emergency conditions, and the most common indicator of a caesarean section is a prior CS. The key contributing factors may include:
- High rates of illiteracy and poverty among women of reproductive age.
- Early marriages.
- High parity.
- More extended average gestational periods.
- Defects in the healthcare system.
The best way to reduce problems from past C-sections is to prevent the first one. This may be done by implementing policies like trying vaginal delivery after past C-sections, selective vaginal delivery of breech babies, regular C-section audits, and early identification of at-risk patients.
|


 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now










