What is the full form of NCPF1. NCPF: National Collection of Pathogenic FungiNCPF stands for National Collection of Pathogenic Fungi. PHE culture collections consist of four collections: ECACC, NCPV, NCTC, and the National Collection Of Pathogenic Fungi (NCPF). More than 4000 strains of fungus and yeast are currently held by NCPF, which was established in 1946 at the London School of Hygiene and Tropical Medicine. The majority of these strains are offered for sale and distribution globally. The collection has relocated to Bristol, where the Mycology Reference Laboratory can validate all themes before sale and dissemination. It is the only collection of pathogenic fungi in the UK, making it a crucial source of material for research. Additionally, the NCPF offers various other services that can be viewed on their website, including training sessions for identifying pathogenic fungi. 
Various vascular liver diseases called NCPH can cause PHT and HVPG that are close to normal. EHPVO is an illness of childhood, whereas NCPF/IPH is a disorder in young adults or middle-aged women. The most likely aetiology is early-onset acute or recurrent infections in a person predisposed to thrombosis. With maintained liver functioning and clinically significant PHT, both diseases occur. The diagnosis is straightforward and is frequently made clinically with the aid of imaging techniques. Control and prevention of variceal bleeding are the main focuses of treatment. Added issues with EHPVO include development retardation, outlet biliopathy, MHE, and parenchymal dysfunction. Patients with endotherapy oversight, exuding from areas not amenable to endotherapy, symptomatic hypersplenism, or symptomatic biliopathy, should consider surgical shunts. Other surgical indications include persistent growth failure, symptomatic and recurring hepatic encephalopathy, decreased quality of life, or significant splenomegaly that interferes with everyday activities. The suggested shunt for EHPVO is Rex-shunt or MLPVB, although these procedures require a thorough pre-operative radiological evaluation and surgical skill. The prognosis for both illnesses is generally favourable, but they require close monitoring regularly. Hepatic schistosomiasis, CHF, and NRH all appear similar and have similar projections. A portal venous strain incline of more than five mmHg between the portal vein (PV) and subordinate vena cava characterizes portal hypertension (PHT), a clinical condition. Because of increased sinusoidal resistance, cirrhotic PHT is linked with an enhanced hepatic venous pressure gradient (HVPG). PHT frequently occurs as an advanced symptom of the underlying condition. 2. Non-cirrhotic Portal Fibrosis (NCPF)NCPF also stands for Non-cirrhotic Portal Fibrosis. Idiopathic PHT (IPH), hepatoportal sclerosis, and obliterative venopathy are other names for Non-cirrhotic Portal Fibrosis (NCPF), a condition with an unidentified aetiology. In two states-non-cirrhotic portal fibrosis (NCPF) and extrahepatic PV obstacle (EHPVO). There is just a PHT-like presentation and no indication of severe parenchymal dysfunction. Researchers will include an updated explanation of these two clinical entities and some additional causes in this review. Non-cirrhotic PHT (NCPH) has an HVPG that is normal or mildly elevated and much lower than PV pressure. The disorders that induce NCPH are predominantly vascular and are physically categorized as pre-, hepatic-, and post-hepatic based on the location of blood flow resistance. Hepatic causes are further split into pre-, sinusoidal-, and post-sinusoidal categories. This is medically indicated by intermediate to enormous splenomegaly, with or without hypersplenism, held liver operations, and patent hepatic and portal veins. 
The disease has been reported nearly worldwide, particularly in originating nations. According to the Asia Pacific Association for the Study of the Liver's (APASL) consensus statement on NCPF, the illness is responsible for 10-30% of all variceal bleed patients worldwide, including in India. Young guys in their third to fourth decades who are members of poor socioeconomic groups are more likely to have it. IPH, also known as idiopathic non-cirrhotic PHT in the West and IPH in Japan, is a condition that resembles NCPF and typically affects women. It often manifests in the fifth decade. Variances may bring about these disparities in the demographics in the living environment, ethnicity, average life expectancy, reporting bias, and diagnostic criteria used. There are theories that the disease's occurrence is declining, which may be related to better prenatal hygiene and care standards, resulting in fewer cases of umbilical sepsis and diarrheal episodes in young children. Animal ResearchThe development of splenomegaly, high portal pressures, and low mean arterial pressures in NCPF mice, along with normal liver function and histology, show the importance of the vascular compartment in PHT. The chronic arsenic exposure animal shows elevated collagen and hydroxyproline levels without appreciable hepatic fibrosis. Radiologic CharacteristicsThe initial line of radiological investigation in both conditions is Doppler USG. The Liver is standard in measure and echotexture in NCPF/IPH. Gamma-Gandy bodies cause the spleen to expand, while NCPF/IPH causes a dilated and patent splenoportal axis. PV has echogenic and denser barriers (>3 mm), and its intrahepatic radicles exist silky and standard. Intrahepatic second and third-degree PV branches abruptly narrow or severed, giving the impression of a "withered tree" and vascular channels approaching one another. PV inflow and splenic index are both high. In 16% of cases, spontaneous shunts (paraumbilical and gastroadrenorenal) are observed. Contrast-enhanced computed tomographies (CT) characteristics, such as intrahepatic PV abnormalities. Non-visualization, reduced calibre, occlusive thrombus, focal nodular hyperplasia, such as nodules, and perfusion deficiencies, aid in the differentiation of NCPF/IPH. Because of cirrhosis. The absence of enhanced bone marrow absorption is shown by radionuclide scintigraphy using 99mTc-Sn colloid. 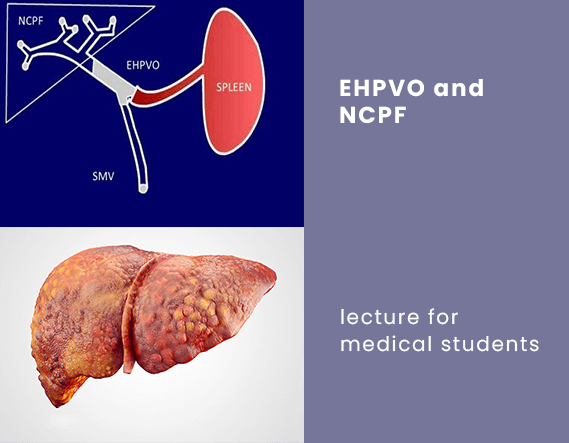
Doppler USG of SPA contains a sharpness and particularity beyond 95% for the diagnosis of EHPVO. PV has undergone cavernomatous change. Splenoportography and arterial portography have been superseded by non-invasive techniques, including CT and MR angiography and portography. In addition to providing a diagnosis, also provide anatomical guidance before shunt surgery. IPH and NCPF/HIVWe should pay particular attention to NCPF/IPH in the context of HIV and AIDS. Approximately 0.45-1 per cent of HIV patients have NCPF/IPH, which is rising quickly. It is because HIV-infected patients live longer after using highly active antiretroviral therapy (HAART), and it's caused by one or more of the following factors: didanosine use, in particular, hypercoagulability, and a direct HIV-related effect. However, the precise mechanism is still unknown. Controversy exists over the function of the underlying prothrombotic condition. As evidenced by its tendency to contaminate hepatic stellate enclosures and cause endothelial damage via cytokines like endothelin-1, HIV may be involved in the disease's aetiology. 1, 6, and platelet-derived growth factors are also mentioned. The prevalence of HIV-related NCPF is primarily male (50-100%), gay (50-75%), long (11.5 years on average, range 7-15 years), and linked to immunological reconstitution. Patients with HIV who develop NCPF are older, have lower CD4 and platelet counts, increased liver enzymes, prolonged didanosine exposure, or both didanosine and stavudine or tenofovir exposure concurrently. The presentation includes PHT features. The range of the Liver's stiffness is 7.8-10.2 kPa. HVPG, on average, is eight mmHg. 25-75% of patients have PVT. It has been documented that liver decompensation necessitates liver transplantation (LTx). NCPF's Natural History and OutlookNearly 100% and 80% of patients experience long-term survival following the removal of esophagogastric varices. Most of the time, liver functions are adequately kept, but 20 to 33% of the time, the Liver slowly experiences parenchymal shrinkage. It leads to decompensation, the development of HPS, and the requirement for LTx. A frequent cause of mortality is uncontrolled variceal bleeding. PVT, ascites, and liver failure were shown to develop in a French follow-up study in 46 per cent, 50 per cent, and 21 per cent of patients, respectively, over a mean period of 7.6 years. The latter two complications were linked to variceal bleeding, surgery, or extrahepatic disease at the same time. PHT deteriorated, and fresh PVT was developed in 46 and 28 per cent of cases, respectively, with some patients requiring LTx. Thus, it is believed that the emergence of PVT is a crucial factor in developing liver disease and final decompensation. However, the transplant and autopsy series did not demonstrate the same. ManagementManaging an acute episode of variceal bleeding is the primary goal of management in both NCPF/IPH and EHPVO, followed by secondary prophylaxis. Splenomegaly, hypersplenism, growth, portal biliopathy, and MHE are additional issues that require attention, the last three in particular in EHPVO. Depending on the age at presentation, the location and kind of obstruction, and the clinical symptoms, EHPVO needs to be managed individually. Medical SupervisionWe should start vasoactive medications such as somatostatin, octreotide, or terlipressin as soon as possible. In one randomized controlled study (RCT) in NCPH, our team conducted propanolol and endoscopic variceal ligation (EVL) were equally effective in preventing rebleeding. In the propranolol group, 47 per cent of varices exhibited a decline in severity, and 18 per cent experienced minimal side effects. Surgical InterventionPatients with variceal bleed who do not respond to endoscopic therapy are often candidates for surgery. Various surgical techniques include: Shunt/Bypass TechniquesNon-physiological shunts entirely or partially bypass the portal blood and enter the systemic circulation. As the latter selectively decompresses the gastrosplenic zone, total and partial shunts are also referred to as selective and non-selective shunts, respectively. While avoiding the level of obstruction, physiological shunts such as the mesenterico-left PV bypass (MLPVB) or Rex shunt maintain the hepatic portal blood flow. An autologous graft relaxes the splanchnic mattress from the significant mesenteric vein to the left stem of the PV (usually the internal jugular vein). 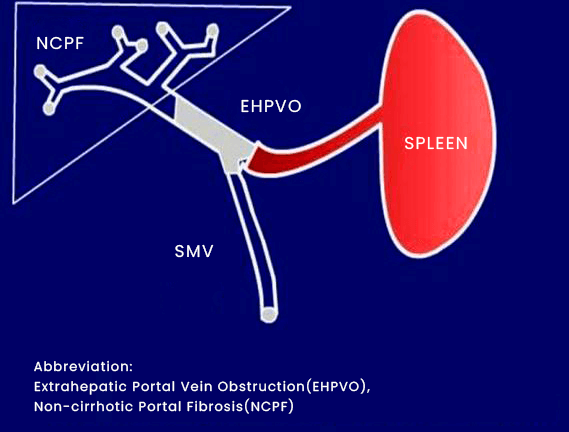
Even though numerous lengthy surgical series on EHPVO, esophageal varices, splenic size, and splenic pulp pressure in NCPF/IPH patients decrease after shunt surgery. However, there is a chance of MHE, glomerulonephritis, pulmonary arteriovenous fistula, and ascites. Concerns with EHPVO include specialized dilemma, shunt thrombosis, rebleeding, and MHE. Advances in surgical procedures have mainly resolved these problems. In terms of patency and decreased rebleeding and encephalopathy rates, particular shunts like the distal splenorenal shunt (DSRS) outperform non-selective ones like the significant (CSRS) or proximal splenorenal shunt (PSRS). Physiological shunts treat the disease or defect, not only the PHT's symptoms and aftereffects. Post-Rex shunt shows improvements in clotting level, development indices, liver importance, spleen size, hypersplenism, reversion of hepatic encephalopathy, and fluid balance. Short-term memory, processing speed, and attention span are neurocognitive abilities. Additionally, MLPVB shields adults from developing liver disease and portal biliopathy. Due to these factors, MLPVB has emerged as the preferred initial surgery in EHVPO cases. For non-selective shunts, a minimum reported doctor's formerly recommended age of one month and a shuntable vein size of 6.5 mm; however, for MLPVB, a vein size of 2 mm is deemed appropriate. Many Root Causes of NCPHThere are various causes of NCPH with a similar appearance in addition to NCPF/IPH and EHPVO. Below is a discussion of three of the typical ones. Schistosoma HepaticaOne of the two trematode flukes, Schistosoma mansoni or japonicum, is responsible for schistosomiasis-related liver damage. While the latter is more typical in eastern Asia, particularly mainland China, the former is more prevalent in Africa and South America. While the latter's larvae live in the superior mesenteric vein, the former's are found in the colonic and rectal tributaries. Egg entrapment in portal venules (50 mm in diameter) results in the development of liver disease. In 4-8% of instances, granulomatous inflammation causes fibrosis (also known as "Symmers pipestem fibrosis"), followed by a presinusoidal rash. Live eggs initially cause a Th1 response with severe granulomatous inflammation, but a Th2 reply later replaces this with the development of fibrosis. Interleukin (IL)-13 positively regulates the deposition of procollagens I, III, and IV and their indicators (fibronectin and glycosaminoglycans), while gamma-interferon negatively regulates it. It has been shown that different proteins associated with stress, immunity, the anti-oxidative response, and structural elements are elevated in schistosomal mouse models. At the same time, those related to various metabolic cycles are decreased . In these livers, the Foxp3 gene, which is required for developing CD4+ CD25+ T reg cells, is overexpressed, improving granuloma formation. A gene is closely related to the HLA-A5 allele and severe disease. NCPF and EHPVO share a similar clinical appearance. Detecting eggs in stools or a rectal biopsy is the basis for the diagnosis, and the Kato-Katz method is used for stool microscopy. The circumoral precipitin test (COPT), alkaline phosphatase immunoassay (APIA), and enzyme-linked immunosorbent assay with the soluble antigen of Schistosoma mansoni eggs using sodium meta periodate (ELISA-SEA-SMP) are serological assays for diagnosis. Sonographically, PV radicles exhibit echogenic thickening and septae that resemble a fish-scale network. A turtle-back look is created by junctional notches, capsular and septal calcifications, uneven hepatic contours, and hypoattenuating bands or rings around the portal tracts, as seen on a CT scan. The quantity of eggs deposited in the Liver, which generally corresponds to the number of eggs expelled in stool, is closely correlated with the natural history of PHT. In untreated patients, PHT begins as presinusoidal and develops perisinusoidal characteristics. In 28.2% of instances, praziquantel treatment results in complete regression of periportal thickness within 3-5 years. Reductions followed them in spleen size and mesenteric and splenic vein width. An artemesinin and praziquantel combination is superior to praziquantel alone, according to a recent meta-analysis. Beta-blockers, surgery, or endotherapy are all options for treating PHT. Esophagogastric devascularization with splenectomy has improved hyperdynamic circulatory status in schistosomiasis patients with lower mortality and complication rates than DSRS.
Next TopicFull Form
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share