What is DVT?
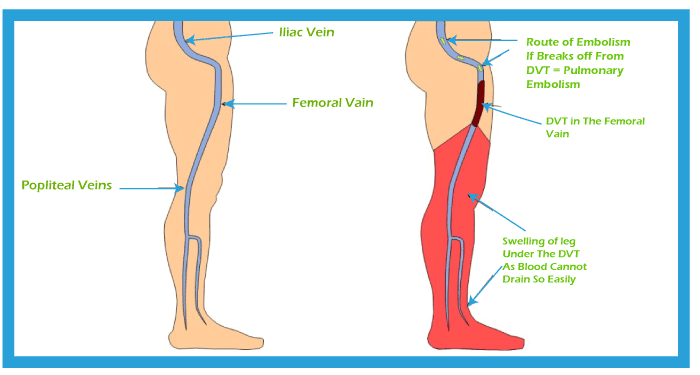
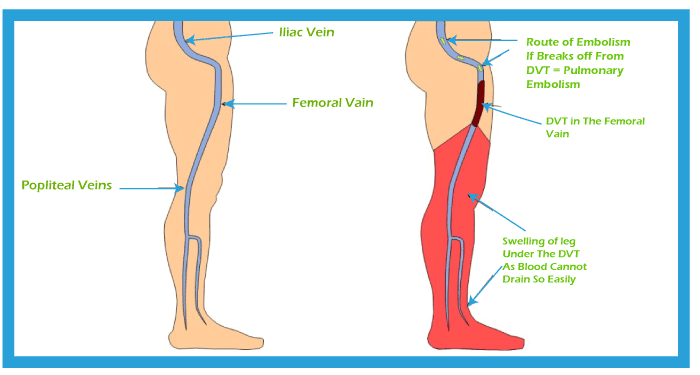
Deep vein thrombosis (DVT) occurs when a blood clot forms in one or more of the deep veins in your body, usually in your legs. A blood clot is a clump of blood that's turned into a solid state. DVT can cause leg pain or swelling and also occur with no symptoms.
You can get DVT if you have certain medical conditions. For example, a blood clot in your legs can happen if you don't move your leg for a long time, such as after surgery or an accident, when you're traveling a long distance, or on bed rest.
Deep vein thrombosis can be severe because blood clots in your veins can break loose, travel through your bloodstream, and get stuck in your lungs, blocking blood flow (pulmonary embolism). However, pulmonary embolism can occur with no evidence of DVT.
When DVT and pulmonary embolism occur together, it's called venous thromboembolism (VTE). Deep Vein Thrombosis and Pulmonary Embolism (DVT/PE) are often severe and underdiagnosed but preventable medical conditions.
Symptoms of DVT
According to the Centers for Disease Control and Prevention (CDC), DVT symptoms only occur in about half of the people who have these health issues. However, here are some common symptoms:
- Swelling in your foot, leg, or ankle, usually on one side.
- Cramping pain in your affected leg usually begins in your calf.
- Severe, unexplained pain in your ankle and foot.
- An area of skin that feels warmer than the skin on the surrounding areas.
- The skin over the affected area turning pale or reddish and bluish color.
People with an upper extremity DVT, or a blood clot in the arm, may also not experience symptoms. Instead, the common symptoms include:
- Neck and shoulder pain
- Swelling in the arm or hand
- Pain that moves from the arm to the forearm
- Weakness in the hand
- Blue-tinted skin color
People may not find out that they have DVT until they've gone through emergency treatment for a pulmonary embolism.
A pulmonary embolism can happen when a DVT clot has moved from the arm or leg into the lung. When an artery in the lung becomes blocked, it's a life-threatening condition and requires emergency care. If a clot dislodges and travels to the lung, the following symptoms may indicate PE:
- Rapid breaths
- Slow breathing or sudden breathlessness
- Chest pain, usually more severe while breathing deeply
- A faster heart rate
How DVT Diagnosed?
If a doctor thinks you have DVT, you should be referred to the hospital within 24 hours for an ultrasound scan. The scan shows whether blood is flowing normally through the vein.
You may also have an X-ray of the vein (venogram). For this, you will be injected with a dye to show where the blood clot is.
DVT Causes and Risk Factor
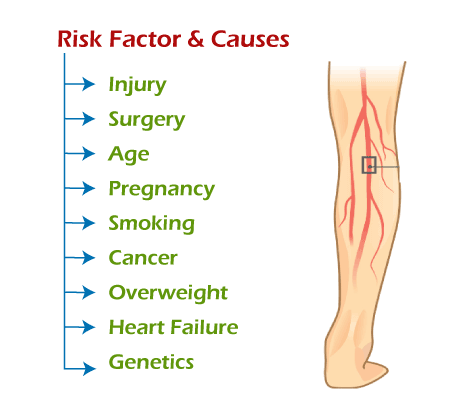
A blood clot causes DVT. The clot blocks a vein, preventing blood from circulating in your body. Clotting may occur for several reasons. These include:
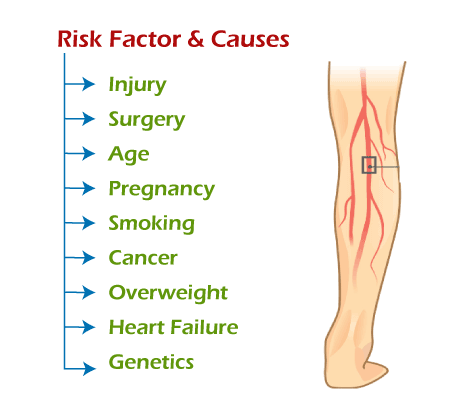
- Injury: Damage to a blood vessel's wall can narrow or block blood flow. A blood clot may form as a result.
- Surgery: Blood vessels can be damaged during surgery, leading to the development of a blood clot. Bed rest with little to no movement after surgery may also increase your risk of developing a blood clot.
- Reduced mobility or inactivity: When you sit frequently, blood can collect in your legs, especially the lower parts. If you're unable to move for an extended time, the blood flow in your legs can slow down. This can cause a clot to develop.
- Certain medications: Some medications increase the chances your blood will form a clot.
- Age: Being older than 60 increases your risk of DVT, though it can occur at any age.
- Sitting for a long time, such as driving or flying: When your legs remain still for hours, your calf muscles don't contract. Muscle contractions usually help blood circulate.
- Prolonged bed rest, such as during a long hospital stay or paralysis: Blood clots can form in the calves of your legs if your calf muscles don't move for long periods.
- Pregnancy: Pregnancy increases the pressure in the veins in your pelvis and legs. Women with an inherited clotting disorder are especially at risk. The risk of blood clots from pregnancy can continue for up to six weeks after you have your baby.
- Birth control pills or hormone replacement therapy: Both can increase your blood's ability to clot.
- Being overweight or obese: Being overweight increases the pressure in the veins in your pelvis and legs.
- Smoking: Smoking affects blood clotting and circulation, which can increase your risk of DVT.
- Cancer: Some forms of cancer increase substances in your blood that cause your blood to clot. Some forms of cancer treatment also increase the risk of blood clots.
- Heart failure: This increases your risk of DVT and pulmonary embolism. Because people with heart failure have limited heart and lung function, the symptoms caused by even a small pulmonary embolism are more noticeable.
- Inflammatory bowel disease: Bowel diseases, such as Crohn's disease or ulcerative colitis, increase DVT risk.
- A personal or family history of DVT or PE: If you or someone in your family has had one or both of these, you might be at greater risk of developing DVT.
- Genetics: Some people inherit genetic risk factors or disorders, such as factor V Leiden, that make their blood clots more easily. An inherited disorder on its own might not cause blood clots unless combined with one or more other risk factors.
- No known risk factor: Sometimes, a blood clot in a vein can occur with any apparent underlying risk factor. This is called an unprovoked VTE.
DVT Prevention
Measures to prevent deep vein thrombosis include the following:
- Avoid sitting still: If you have had surgery or have been on bed rest for other reasons, try to get moving as soon as possible. When sitting for a long time, such as during traveling for more than four hours, then do:
- Exercise your legs while you're sitting by:
- Raising and lowering your heels while keeping your toes on the floor
- Raising and lowering your toes while keeping your heels on the floor
- Tightening and releasing your leg muscles
- Wear loose-fitting clothes.
- Get up and walk around every 2 to 3 hours.
- Don't cross your legs, which can block blood flow.
- Stop smoking:Smoking increases your risk of getting DVT.
- Exercise and manage your weight: Obesity is a risk factor for DVT. Regular exercise lowers your risk of blood clots, especially for people who sit a lot or travel frequently.
- Maintaining pressure on the at-risk area:This can prevent blood pooling and clotting. Medical professionals may recommend wearing compression stockings or a boot that fills with air to increase pressure.
- Anticoagulant medication: A doctor may prescribe blood-thinning medication to reduce the risk of clotting before or after surgery.
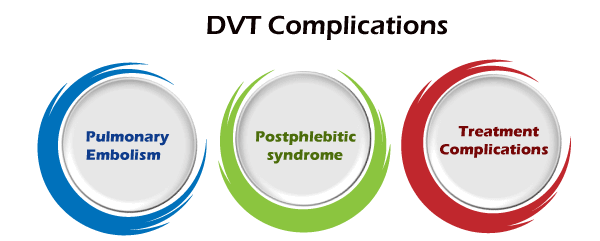
DVT Complications
DVT have the complications that patients may be faced, such as:
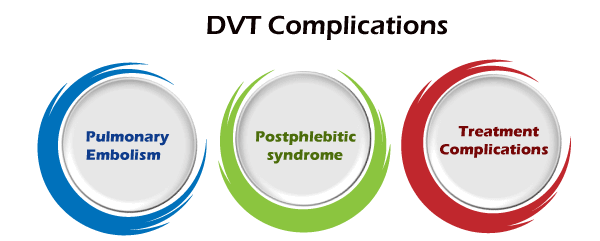
- Pulmonary embolism (PE):PE is a potentially life-threatening complication associated with DVT. It occurs when a blood vessel in your lung becomes blocked by a blood clot that travels to your lung from another part of your body, usually your leg.
It's essential to get immediate medical help if you have signs and symptoms of PE. For example, sudden shortness of breath, chest pain while inhaling or coughing, rapid breathing, rapid pulse, feeling faint or fainting, and coughing up blood may occur with a PE.
- Postphlebitic syndrome: Damage to your veins from the blood clot reduces blood flow in the affected areas, causing leg pain and swelling, skin discoloration, and skin sores.
- Treatment complications: Complications may result from blood thinners used to treat DVTs. Bleeding is a problematic side effect of blood thinners. It's essential to have regular blood tests while taking such medications.
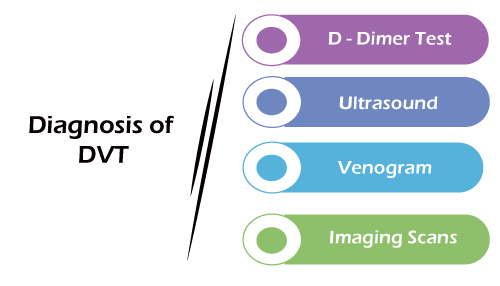
Diagnosis of DVT
If a person suspects that they may have DVT, they should seek immediate medical attention. The doctor will ask questions about symptoms and medical history before carrying out a physical examination.
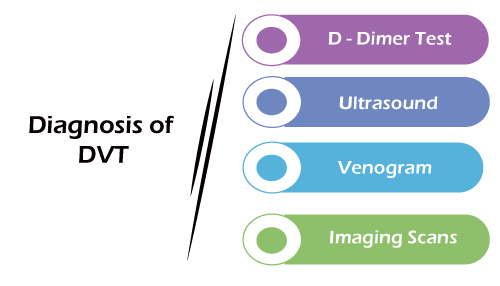
A doctor will usually not be able to diagnose DVT through symptoms alone and may recommend tests, including:
- D-dimer Test: D-dimer is a protein fragment present in the blood after a blood clot fibrinolysis degrades a blood clot. A test result revealing more than a certain amount of D-dimer indicates a possible blood clot. However, this test may not be reliable in individuals with certain inflammatory conditions and after surgery.
- Ultrasound: Ultrasound is the standard method of diagnosing the presence of DVT. This type of scan can detect clots in veins, alterations in blood flow, whether the clot is acute or chronic, where it is located in the leg or arm, and how large it is.
If necessary, ultrasounds may be compared over time to see whether a clot has grown or resolved. Clots in the chest or pelvis may not be identified on ultrasound.
- Venogram: A doctor may request this scan if the ultrasound and D-dimer tests do not provide enough information. The doctor injects a dye into a vein in the foot, knee, or groin. X-ray images can track the dye as it moves to reveal the location of a blood clot.
- Other imaging scans: MRI and CT scans may highlight the presence of a clot. These scans may identify blood clots while testing for other health conditions.
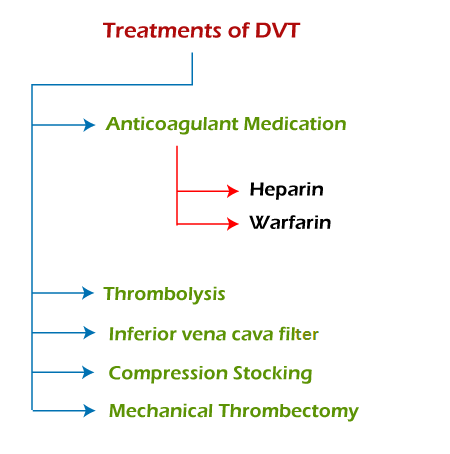
Treatments of DVT
DVT treatment aims to stop the growth of a clot, prevent a clot from becoming an embolism and moving into the lung. It reduces the risk that DVT might come back after treatment and minimize the risk of other complications.
A doctor may recommend several methods to manage DVT, such as:
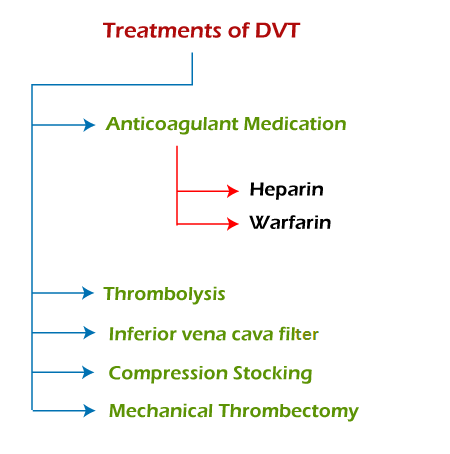
1. Anticoagulant medications
These are drugs that prevent the clot from growing, as well as reducing the risk of embolism. These two types of anticoagulants support the treatment of DVT:
- Heparin: Heparin has an immediate effect. For this reason, doctors usually administer it first through a brief course of injections lasting less than a week.
- Warfarin: The doctor is likely to recommend a 3-6-month course of oral tablets to prevent recurrence of DVT.
People with recurrent DVT may need to take anticoagulant medication for the rest of their lives.
2. Thrombolysis
People with more severe DVT or PE require immediate medical attention. The doctor or emergency team administers drugs called thrombolytics, or clot busters, that break down clots. Tissue plasminogen activator (TPA) is an example of a thrombolytic drug.
Excessive bleeding is a side effect of these drugs. As a result, medical teams only administer TPA or similar interventions in emergencies.
Healthcare professionals administer TPA through a small catheter or tube directly into the clot's site. Patients undergoing catheter-directed thrombolysis will be in the hospital for several days and have intermittent lysis checks to make sure the clot is breaking down appropriately.
3. Inferior vena cava filter
A surgeon inserts a tiny device resembling an umbrella into the vena cava, a large vein. The device catches blood clots and stops them from moving into the lungs while allowing blood flow to continue.
4. Compression stocking
People wear these to help reduce pain, limit swelling, and prevent ulcers from developing. Stockings can also protect the individual from the post-thrombotic syndrome. Someone with DVT will have to wear stockings at all times for at least 24 months.
5. Mechanical thrombectomy
This is a relatively new technique that surgeons may use to treat a blood clot with DVT or PE. The procedure involves using a catheter and a clot-removing device, an aspiration catheter, a retrieval stent, or a pump. Using imaging techniques for guidance, the surgeon:
- Inserts the catheter toward the area where the clot exists.
- Directs the clot-removing device through the catheter.
- Removes the clot using aspiration or a stent and reestablishes blood flow.
The authors of a 2019 review concluded that mechanical thrombectomy is safe and effective at treating DVT and reducing the risk of recurrence.
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now










