What is MS in Medical Terms?Multiple sclerosis or MS is a chronic disease of the central nervous system (CNS), which means the brain and spinal cord. In MS, the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between the brain and the rest of the body. This disease can cause temporary, repetitive, sustained disruptions, permanent damage, or deterioration of the nerves. Signs and symptoms of MS vary widely and depend on the amount of nerve damage and which nerves are affected. Some people with severe MS may lose the ability to walk independently or at all, while others may experience long periods of remission without any new symptoms. Unfortunately, there's no cure for multiple sclerosis. However, treatments can help speed recovery from attacks, modify the course of the disease, and manage symptoms. The clinical picture in MS depends upon the extent of demyelination. Multiple sclerosis is a relatively common disorder: more than 400,000 Americans are affected, of whom the majority (about 390,000) are adults. Multiple sclerosis usually begins between ages 20 and 40. Women are twice as likely to have the disease as men, and European-Americans are more likely to be affected than African-Americans or Asian-Americans. About half of all patients with MS become unable to work within 10 to 15 years of the first onset of symptoms. Within 25 years of the first symptoms, half of these patients cannot walk. Symptoms of MSMultiple sclerosis signs and symptoms may differ significantly from person to person and throughout the disease, depending on the location of affected nerve fibers. In addition, symptoms often affect movement, such as:
Symptoms of multiple sclerosis may be single or multiple. They may range from mild to severe in intensity. They may also be long-term or short-term in duration. Multiple sclerosis symptoms may also include:
Types of MSMS is classified into four main types by the National MS Society Advisory Committee on Clinical Trials in MS. The types are based on the phase and severity of disease progression. The categories are important because they help predict how severe the disease can be and how well treatment will work. 
1. Clinically Isolated Syndrome (CIS) CIS is the first episode of neurologic symptoms caused by inflammation and demyelination in the central nervous system. By definition, the episode must last for at least 24 hours, is characteristic of multiple sclerosis but does not yet meet the criteria for a diagnosis of MS because people who experience a CIS may or may not develop MS. When lesions accompany CIS on a brain MRI that is similar to those seen in MS, the person has a high likelihood of the second episode of neurologic symptoms and diagnosis of relapsing-remitting MS. Conversely, when CIS is not accompanied by MS-like lesions on a brain MRI, the person has a much lower likelihood of developing MS. 2. Relapsing-remitting MS (RRMS) RRMS is the most common form of multiple sclerosis. It is characterized by clearly defined attacks of new or increasing neurologic symptoms. These attacks are also called relapses or exacerbations. They are followed by periods of partial or complete recovery (remissions). During remissions, all symptoms may disappear, or some symptoms may continue and become permanent. However, there is no apparent progression of the disease during the periods of remission. RRMS can be further characterized as either active (with relapses and evidence of new MRI activity over a specified time) or not active, as well as worsening (a confirmed increase in disability following a relapse) or not worsening. Approximately 75 to 85 % of people with MS are initially diagnosed with RRMS. 
This graphic shows the kinds of disease activity that can occur in RRMS over time; however, each person's experience with RRMS will be unique. 3. Primary progressive MS (PPMS) PPMS is characterized by worsening neurologic function (accumulation of disability) from the onset of symptoms, without early relapses or remissions. PPMS can be further characterized as either active (with an occasional relapse or evidence of new MRI activity over a specified time) or not active, as well as with progression (evidence of disability accumulation over time, with or without relapse or new MRI activity) or without progression. Approximately 15 percent of people with MS are diagnosed with PPMS. 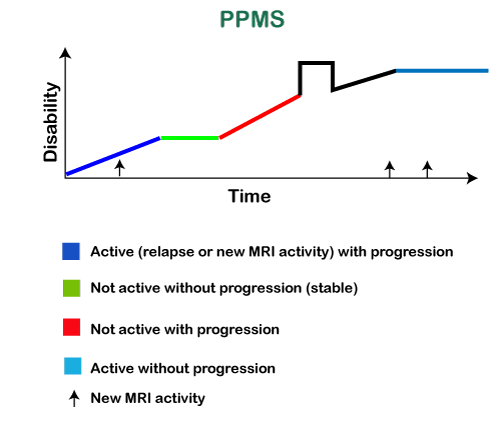
This graphic shows the kinds of disease activity that can occur in PPMS over time; however, each person's experience with PPMS will be unique. PPMS can have brief periods when the disease is stable, with or without a relapse or new MRI activity, and periods when increasing disability occurs with or without new relapses or lesions on MRI. 4. Secondary progressive MS (SPMS) SPMS follows an initial relapsing-remitting course. However, some people diagnosed with RRMS will eventually transition to a secondary progressive course in which there is a progressive worsening of neurologic function (accumulation of disability) over time. SPMS can be further characterized as either active (with relapses and evidence of new MRI activity during a specified time) or not active, as well as with progression (evidence of disability accumulation over time, with or without relapses or new MRI activity) or without progression. 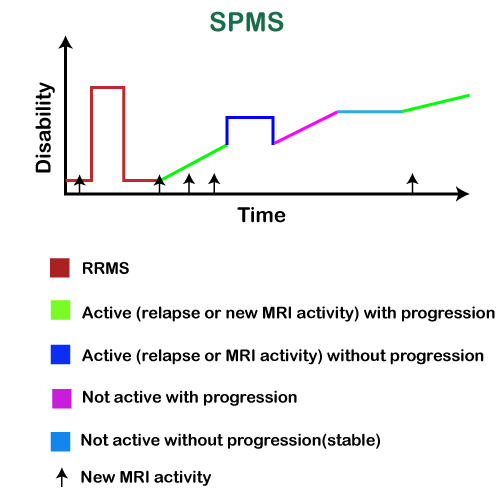
This graphic shows the kinds of disease activity that can occur in SPMS over time; however, each person's experience with SPMS will be unique. SPMS follows after relapsing-remitting MS. Disability gradually increases over time, with or without evidence of disease activity (relapses or changes on MRI). In SPMS, occasional relapses may occur, as well as periods of stability. Risk Factors of MSThese factors may increase your risk of developing multiple sclerosis:
Causes of MSWe don't know exactly what causes multiple sclerosis, but it is believed to be some combination of immunologic, environmental, infectious, or genetic factors. Some theories have been proposed, though there is not enough evidence to establish any one cause. Theories as to what causes MS include:
How to Diagnose MS?There are no specific tests for MS. Instead, a diagnosis of multiple sclerosis is often challenging to diagnose as symptoms are so varied and can resemble other diseases. Therefore, it is often diagnosed by process of exclusion, such as:
The doctor will start by asking you about your medical history and your symptoms. They'll also do a few tests to see if your brain and spinal cord are working as they should. These include:
In most people with relapsing-remitting MS, the diagnosis is quite straightforward and based on a pattern of symptoms consistent with the disease and confirmed by brain imaging scans, such as MRI. Diagnosing MS can be more difficult in people with unusual symptoms or progressive disease. Further testing with spinal fluid analysis, evoked potentials, and additional imaging may be needed in these cases. Multiple Sclerosis TreatmentThere is no cure for multiple sclerosis. Treatment typically focuses on speeding recovery from attacks, slowing the progression of the disease, and managing MS symptoms. Some people have such mild symptoms that no treatment is necessary.
Next TopicWhat is PAC
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share









