Blood BankA blood bank is a facility where blood collected through blood donation is kept and maintained for future use in blood transfusions. A blood bank is a term used to refer to that portion of the hospital where the blood samples are stored, and appropriate Blood testing is done to reduce the risk of transfusion-related mis happenings. 
However, it may also refer to a collection facility that some hospitals have. The blood banking process includes several steps like collecting blood followed by processing the collected blood, testing, separating, and storing the blood. Types Of Blood TransfusionsSeveral types of blood transfusion exist:

The Platelet transfusion procedure is more favourable for patients with a severe infection, burns, or liver failure. The plasma can be stored frozen for around 12 months at minus 25 degrees Celsius. Plasmapheresis is the separation of plasma from donor blood. HistoryThe history of blood bank formation comes with the discovery of anticoagulant compounds that can help in blood storage. It has always been known that blood can be transfused between donor and receiver before it gets coagulated. But with the discovery of anticoagulant compounds and refrigerating the blood, people started storing blood for many days, resulting in forming different blood banks. It all started in the late 1800. John Braxton Hicks was the first person to invent a distinct chemical procedure to stop blood coagulation at Saint Mary's Hospital in London. However, his experiments using phosphate in soda were futile. 
On March 27, 1914, Belgian doctor Albert Hustin performed the first non-direct transfusion. However, it was a diluted solution of blood. During the same year in November, another doctor from Argentine, Luis Agote, discovered a significantly less diluted solution. Both the doctors relied on the chemical compound sodium citrate to use as an anticoagulation compound. First World WarThe rapid development of a large number of blood banks came during the first world war. Lieutenant Lawrence Bruce Robertson of Canada played an important role in convincing the royal Army medical corpse to adopt the transfusion of blood method at casualty clearing stations for the injured army men. 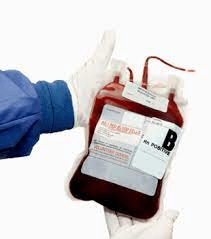
In October 1915, Robertson conducted his first wartime syringe transfusion on a patient with numerous shrapnel wounds. As the months passed, more blood transfusions were carried out, and the success of careful blood transfusion was reported to Sir Walter Morley Fletcher. He was the director of the Medical Research Committee. At the time around 1916, Robertson first published his studies on blood transfusion in the British Medical Journal and was successful in inclining the attention of British authorities toward the method of blood transfusion and its benefits at that time. Robertson got favoured by a few like-minded individuals like the eminent physician Edward William Archibald who helped him pursue the British authorities. Robertson constructed the first blood bank transfusion system in the spring of 1917 at the casualty care station on the Western front. Another medical researcher, a US army officer, Oswald hope Robertson, was sent to the RAMC, where he was made an important person in managing the first blood bank. He used troops as blood donors to prepare for the anticipated third Battle of Ypres. At this time, sodium citrate was used as an anticoagulation compound. The blood was collected with the help of vein punctures, and all the collected blood was kept and stored in bottles at British and American casualty clearing stations along the front. He also tried storing isolated red blood cells in chilled bottles. Geoffrey Keynes, a British physician, invented a portable system to store blood, allowing easier transfusions. ExpansionIn 1925, Alexander Bogdanov created a scientific centre in Moscow to study the effects of blood transfusion. Percy Oliver, secretary of the British Red Cross, founded the world's first blood donation program in 1921. 
Blood transfusion service in London was very rapidly developed and was freely available. A battery of physical tests was administered to volunteers to determine their blood type. Around 1925 the service served approximately 500 patients, and the British Red Cross system finally adopted it in 1926. Similar systems were formed in other towns such as Sheffield, Manchester, and Norwich, and the work of the service gained international notice. Different ways of blood transfusion developed in different nations. For example, in the Soviet Union, recently deceased people were used as donors for the transfusion of cadaveric blood. Vladimir Shamov and Sergei Yudin introduced this technique. Yudin executed the successful first transfusion of blood by this method on March 23, 1930. It is followed by presenting the results at the Fourth Congress of Ukrainian Surgeons in Kharkiv. The presentation was on the first 7 clinical transfusions with cadaveric blood transfusions. The blood bank, which became the model for developing other blood banks throughout the Soviet Union, was also developed by Yudin. Around 1930 he developed the world's first blood bank at Nikolay Institute. After this, many blood banks were established in other countries surrounding the Soviet Union. By the mid-1930s, the Soviet Union had established a network of at least 65 big blood facilities and over 500 minor ones, all of which stored "canned" blood and shipped it to all parts of the nation. During the Spanish Civil War in 1936, Frederic Durán-Jordà developed one of the first blood banks. Duran joined the Barcelona Facility's Transfusion Service at the outset of the conflict, but the hospital was quickly overwhelmed by the demand for blood and the scarcity of suitable donors. Duran built a blood bank for injured troops and civilians with the help of the Spanish Republican Army's Department of Health. In a modified Duran Erlenmeyer flask, 300-400 ml (about 13.53 oz) of extracted blood was combined with a 10% citrate solution. The blood was kept at 2 °C in a sterile glass sealed under pressure. During 30 months of operation, the Barcelona Transfusion Service enrolled about 30,000 donors and processed 9,000 litres of blood. Bernard Fantus, head of the therapeutics at Chicago's Cook County Hospital, founded one of the earliest hospital blood banks in the United States in 1937. Fantus coined the term "blood bank" when he established a hospital laboratory that conserved, cooled, and stored donor blood. Hospital and community blood banks sprung up across the country within a few years. 
Throughout the war, the British used to supply military forces with blood from centralized depots, as opposed to the tactic used by the Americans and Germans, who bled men at the front to give essential blood. The British procedure proved to be more effective in achieving all requirements, and over 700,000 donors (about half the population of Hawaii) were bled throughout the war. This method grew into the National Blood Transfusion Service, the first national service founded in 1946. Medical ProgressIn 1940, the United States began a blood collecting program, and Edwin Cohn pioneered the procedure of blood fractionation. He devised methods for separating the serum albumin component of blood plasma, which is critical for maintaining osmotic pressure in blood vessels and preventing them from collapsing. 
Gordon R. Ward invented the use of blood plasma instead of red blood cells. He replaced the method of whole blood transfusion with blood plasma transfusion. Liquid plasma was utilized in Britain during the start of World War II. A big work started in New York city hospitals known as "blood for Britain". The blood was collected from the hospitals for shipping the plasma to Britain. A dry plasma package was created, which minimized breakage and simplified transportation, packing, and storage. The dried plasma bundle was delivered in two tin cans holding 400 cc bottles. One bottle held enough distilled water to rehydrate the dried plasma in the other bottle. The plasma would be ready to use in approximately three minutes and lasted around four hours. Charles R. Drew was named medical supervisor and successfully turned the test tube procedures into the first effective mass production system. In 1939-40, Karl Landsteiner, Alex Wiener, Philip Levine, and R.E. Stetson established the Rhesus blood group system, which was the source of most transfusion responses up to that point. Three years later, J.F. Loutit and Patrick L. Mollison introduced acid-citrate-dextrose (ACD) solution, which lowered the volume of anticoagulants, allowed for larger blood transfusions, and longer-term storage. Around the 1950s, Carl Walter and W.P. Murphy jr invented plastic bags for collecting blood samples. It was a remarkable thing because it replaced the breakable glass bottles. The plastic bags were easily carried and transported across places and were comparatively stronger. This collecting method was safer and easier, and it evolved into the whole blood collection unit of the blood bank. An anticoagulant preservative, CPDA-1, launched in 1979, extended the shelf life of stored blood by up to 42 days (about 1 and a half months), increasing blood supply and facilitating resource sharing across blood banks. Processing And CollectionCertain requirements have been defined for collecting and processing each blood product. The term "whole blood" (WB) refers to a specific product, unseparated venous blood, with an authorized preservative added. Most of the transfusion blood is obtained as whole blood. When RBC units are buffered with glycerol, they can be frozen, although this is a costly and time-consuming method that is seldom used. Frozen red cells have an expiry date of up to 10 years and are preserved at 85 degrees Fahrenheit (65 degrees Celsius). 
The less-dense blood plasma is processed into several frozen components and labelled accordingly depending on when it was frozen, and the product's intended usage. Fresh frozen plasma is often labelled if the plasma is frozen quickly and is intended for transfusion. If it is used to make other goods, it will be labelled as recovered plasma or plasma for fractionation. Other plasma components can be used to create cryoprecipitate. These components must be kept at 0 °F (18 °C) or colder but are usually kept at 22 °F (30 °C). The buffy coat is the covering between red cells and plasma occasionally removed to create platelets for transfusion. Platelets are normally pooled before transfusion and have a shelf life of 5 to 7 days, or 3 days after the institution from where they were acquired has finished their testing. Platelets must be rocked/agitated when kept at room temperature (72 °F or 22 °C). They are highly vulnerable to bacterial growth since they are maintained at room temperature in nutritional solutions. Plasma is the most often obtained component using plasmapheresis; however, red blood cells and platelets can also be collected. Some blood banks also use apheresis to harvest products. These items have the same shelf life and storage requirements as their conventionally manufactured counterparts. Donors are occasionally compensated; in the United States and Europe, most blood for transfusion is obtained from volunteers, but plasma for other reasons may be collected from paid donors. 
Most collection facilities and hospital blood banks also screen patients' blood types and identify suitable blood products, in addition to a battery of tests (e.g., illness) and treatments (e.g., leukocyte filtration) to assure or improve quality. The increasingly acknowledged issue of poor transfusion effectiveness elevates the profile of RBC viability and quality. Notably, hospitals around the world spend more on dealing with the repercussions of transfusion-related issues than on the total cost of purchasing, testing/treating, and transfusing blood. Storage And AdministrationRoutine blood storage is 42 days (about 1 and a half months) or 6 weeks (about 1 and a half months) for stored packed red blood cells (also known as "StRBC" or "pRBC"). This is the most prevalent blood product that is transfused, and entails refrigeration but not freezing. There is a growing debate on whether the age of a given product unit affects transfusion effectiveness, specifically if "older" blood directly or indirectly raises the risk of problems. 
Different studies were conducted to answer these questions, but none proved that older blood is indeed less effective. Mixed results were found, which showed that there might be no difference in older and new blood effectiveness. In contrast, the other studies stated that older blood is less effective. But the storage time was the only possible way to estimate the stored blood's quality. Therefore, the first-in, first-out inventory management approach is currently standard. It is also crucial to note that storage outcomes vary amongst donors, which, paired with limited accessible quality testing, presents hurdles to doctors and regulators seeking dependable indications of quality for blood products and storage systems. Platelet transfusions are significantly less common, yet they provide distinct storage/management challenges. Platelets can only be held for 7 days due to their higher risk for contamination caused by a higher storage temperature. Lesion Of RBC StorageInadequate transfusion effectiveness can come from red blood cell (RBC) blood product units that have been damaged by a storage lesion. A storage lesion is a collection of biochemical and biomechanical changes that occur during storage. This can reduce red cell viability and capacity to oxygenate tissues. Although certain biochemical changes are reversible following blood transfusion, however, biomechanical modifications are not, and rejuvenation products are not yet capable of reversing this phenomenon satisfactorily. Lesion Of Platelet StoragePlatelet storage lesion differs from RBC storage lesion, owing to the varied roles of the products and the distinct aims of the respective transfusions, as well as different processing challenges and inventory management considerations. Different Inventory and Release ProceduresAlthough, as previously stated, the basic inventory-management technique is first-in, first-out (FIFO) to reduce product expiry. However, there are various departures from this policy, both in current practice and under investigation. 
To "guarantee" optimum cell activity, exchange transfusion of RBC in newborns requires using a blood product that is five days old or less. In addition, certain hospital blood banks will try to meet physicians' demands for low-aged RBC products for specific types of patients (e.g., cardiac surgery). Recently, various techniques to supplement or replace FIFO have been investigated. One is to strike a compromise between lowering the average product age (at transfusion) and the requirement to maintain enough supply of non-outdated goods, resulting in a strategic mix of FIFO and last-in, first-out (LIFO). Long-Term PreservationCompared to routine/short-term storage, "long-term" storage for all blood products is unusual. Red blood cells are cryopreserved to hold uncommon units for up to 10 years. The cells are incubated in a glycerol solution, which serves as an antifreeze ("cryoprotectant") within the cells. The glycerol content determines the precise temperature. The units are then stored in special sterile containers in a cold freezer.
Next TopicBlood And Its Components
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










