Lumbar Disk Disease
A vital part of the human vertebral column, specifically in the lumbar region of the spine, is the lumbar disc, also known as the intervertebral disc or spinal disc. This area, which is in the lower back, carries a sizable portion of the body's weight and is prone to deterioration over time. Lumbar discs are essential for maintaining spinal stability, protecting the vertebrae, and enabling the flexibility needed for a variety of movements of the body.
Composition of Lumbar Disk
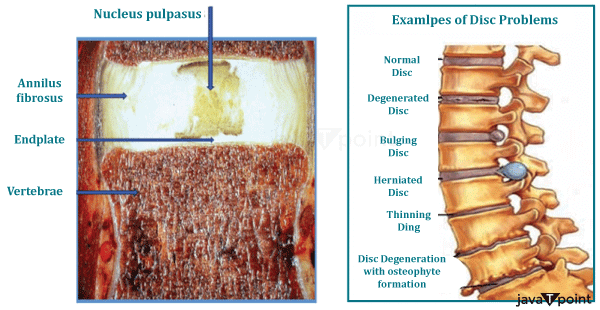
Lumbar discs are made up of two main parts, each of which has unique characteristics and capabilities:
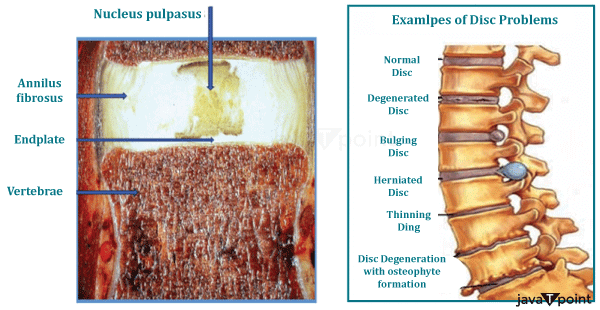
Annulus fibrosus- The lumbar disk's tough, fibrous exterior layer is known as the annulus fibrosus. Like the rings on a tree trunk, the annulus fibrosus is constructed of numerous concentric layers of fibrous tissue. These layers, oriented in different directions, give the disc strength and stability. The strength of the annulus fibrosus is primarily due to its collagen fibres.
Nucleus pulposus- The inner core of the lumbar disc, which is surrounded by the annulus fibrosus, is known as the nucleus pulposus. Its high water content-which can be anywhere between 65% and 85% water-gives it a special gel-like uniformity. Proteoglycans and a web of collagen fibers make up this gel-like substance. The nucleus pulposus's viscous properties, which allow it to contract and expand as needed, are contributed to by the proteoglycans.
Characteristics of Lumbar Disk
The following characteristics set the lumbar intervertebral discs apart:
- Size: When compared to other spinal regions, the lumbar intervertebral discs are the thickest. Additionally, the discs are thicker in front than in back.
- Height: The lumbar discs get smaller throughout the day due to the burden placed on the upper body. According to estimates, the discs can regain their original shape after sleeping for at least 5 hours.
- Shape: The lumbar disc's shape changes as you move. The height of the disc in the front is reduced while the height in the back is increased when the spine bends forward. When bending backwards, the opposite takes place.
Functions of Lumber Disk
In the human body, the lumbar discs perform several vital tasks, including:
- Shock Absorption: Lumbar discs serve as the spine's shock absorbers. The lumbar discs absorb the impact forces produced by movements like walking, running, or lifting, preventing the forces from being transferred directly to the vertebrae. The spine is shielded from excessive wear and tear by this cuffing effect.
- Flexibility and movement: Lumbar discs are crucial in promoting the lumbar spine's flexibility. They enable motions like bending sideways, backwards, and forward. The ability to move freely is necessary for carrying out daily tasks and maintaining good posture.
- Load Distribution: A significant amount of the body's weight is supported by the lumbar region of the spine. To avoid placing undue strain on any one vertebra, lumbar discs assist in evenly distributing this weight across the spine's bones.
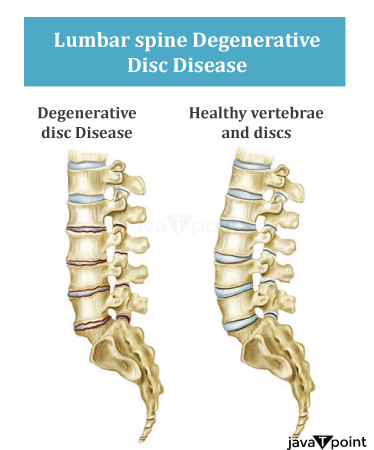
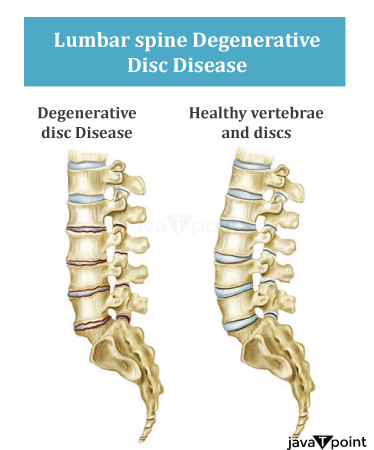
Lumbar Disk Disease
The lumbar region of the spine is affected by lumbar disc disease, also known as lumbar disc disease or intervertebral disc disease. This condition is common and frequently incapacitating. The soft, cushion-like intervertebral discs, which are situated between the lower back's vertebrae, exhibit a variety of degenerative changes that define it. Numerous symptoms and side effects of lumbar disc disease can have a serious negative impact on a person's quality of life.
Causes of the Disease
- Genetics: One's likelihood of developing lumbar disc disease may be increased by afamily history of the condition.
- Trauma: Repeated or severe injuries to the lumbar spine can hasten the degeneration of the intervertebral discs.
- Obesity: Carrying around extra weight can put more strain on the lumbar discs, potentially hastening their deterioration.
- Workplace Risk Factors: Jobs that require heavy lifting, frequent bending, or extended periods of sitting may raise your risk of developing lumbar disc disease.
- Smoking: Smoking is linked to decreased blood flow to the discs, which may hasten the degeneration of those structures.
Symptoms of the Disease
- Lower Back Pain: A defining symptom is lower back pain that is constant and frequently chronic. The discomfort may be dull, aching, or sharp, and it may get worse when you move.
- Leg Pain: Lumbar disc disease can result in the compression or irritation of spinal nerves, which can cause pain to radiate down one or both legs. Sciatica is a condition that can make you feel like you're burning, tingling, or are numb.
- Weakness and Numbness: Some people may have weakness and numbness in their legs, which makes it difficult to go about their daily lives.
- Movement-Induced Pain: Activities that require bending, twisting, or lifting frequently cause pain to become more intense.
- Reflex loss: Severe lumbar disc disease cases can result in the loss of reflexes in the affected leg.
- Bowel or Bladder Dysfunction: In serious instances of lumbar disc disease, particularly when a significant disc herniation compresses the spinal cord, there may be a loss of control over bowel or bladder function. This is a medical emergency that needs to be handled right away.
- Movements and Positions that Can Make Pain Worse: Lumbar disc disease-related pain can be made worse by movements and positions. The discomfort can be made worse by actions like bending forward or lifting heavy objects.
- Rest: Rest can temporarily relieve lower back pain brought on by lumbar disc disease. But when one resumes daily activities, the pain frequently returns.
- Modifications in Walking Pattern: Muscle tremors and pain brought on by lumbar disc disease can cause alterations in a person's gait. Others might notice this changed gait.
- Balance Issues: People with lumbar disc disease may find it difficult to keep their balance due to a combination of muscle weakness and pain, which raises their risk of falling.
- Pain Spreading to Other Areas: Lumbar disc disease occasionally results in pain spreading to other body parts, including the hips, groyne, or even the upper back. Diagnosis may become more difficult as a result.
Diagnosis of Lumber Disk Disease
These are the essential procedures and techniques for diagnosing lumbar disc disease:
- Medical History: A thorough medical history is frequently the first step in the diagnostic process. Your doctor will inquire about your symptoms, their duration, and any pertinent underlying diseases or prior injuries. A thorough history can offer insightful information about the potential causes of your symptoms.
- Physical Exam: A physical exam is performed to evaluate your general health and spot any physical symptoms of lumbar disc disease. The doctor performing the examination might look for sensory changes, reflexes, and muscle weakness in the affected area.
- Neurological Assessment: A neurological assessment is essential because lumbar disc disease can impair nerve function. Tests of muscle power, reflex evaluations, and evaluations of lower limb sensation may be part of this process. Any abnormalities discovered may point to nerve irritation or compression.
Imaging Research:
X-rays offer a basic view of the spine and can be used to spot problems like bone spurs or abnormal spine curvature. They are less successful at detecting soft tissue issues like herniated discs, though.
The most popular and reliable imaging method for detecting lumbar disc disease is MRI (Magnetic Resonance Imaging). The spinal discs, nerves, and surrounding structures are all produced in fine detail. Disc herniations can be precisely located, measured, and graded using MRI technology.
A CT (Computerised Tomography) scan can be used when an MRI is not appropriate or when more precise images of the bone structures are required.
- Electrodiagnostic Tests: In some circumstances, electrodiagnostic tests like nerve conduction studies (NCS) and electromyography (EMG) may be performed to evaluate nerve function and identify the site of nerve compression.
- Discography: To determine the cause of pain, contrast dye is injected into the injured disc during this invasive diagnostic procedure. When other imaging tests are unreliable or when surgery is being considered, it is typically used.
- Clinical Evaluation: A combination of a patient's medical history, physical examination, and imaging tests is frequently used to confirm the diagnosis of lumbar disc disease. The healthcare professional will evaluate the patient's overall clinical situation and choose the most appropriate course of action.
It's crucial to remember that, even though imaging tests like MRI are useful tools, they should be interpreted considering the patient's clinical presentation. The severity of the symptoms and the patient's overall health should be considered when deciding what course of action to take. Not all disc abnormalities detected by imaging necessarily correspond to symptoms.
Treatment of the Disease
- Management of Pain: Pain control should be the priority. Non-steroidal anti-inflammatory drugs (NSAIDs), for example, are over-the-counter drugs that can help reduce pain and inflammation. In cases where the pain is severe, presrciption muscle relaxants may also be considered.
- Physical Therapy: In the management of lumbar disc disease, physical therapy is crucial. Therapists design individualized exercise programmes to strengthen the back and core muscles, enhance flexibility, and improve posture. Recurrent herniations may become much less likely as a result.
- Heat and Cold Therapy: Using heat or cold packs can reduce pain and inflammation momentarily. While cold soothes the area and lessens inflammation, heat eases tension in the muscles and enhances blood flow.
- Epidural steroid injections: These can be used to relieve pain and reduce inflammation in situations where there is severe pain or inflammation. Usually, these injections are used when more conservative measures fall short.
- Minimal Invasive Procedure: Percutaneous discectomy and endoscopic discectomy are two minimally invasive procedures that may be considered if more conservative therapies are unsuccessful in relieving your symptoms. With little disruption to the surrounding tissue, these procedures involve removing or constricting the disc's herniated area.
- Lifestyle Changes: Patients are encouraged to make lifestyle adjustments that support spinal health, such as maintaining a healthy weight, adopting good ergonomics, and staying away from activities that aggravate symptoms.
- Nutrition and supplements: For the health of your bones and discs, you need a diet rich in calcium and vitamin D. For those who have dietary deficiencies, supplements may be suggested.
- Psychological Support: Anxiety and depression are side effects of chronic pain. Patients who need psychological support, such as therapy or counselling, can better manage the emotional difficulties brought on by lumbar disc disease.
Surgical Options
When conservative therapies and minimally invasive techniques are ineffective or when neurological deficits are severe or progressing, surgery is frequently considered.
Following are some surgical remedies for lumbar disc disease:
- portion of the disc in a microdiscectomy. While preserving as much of the healthy disc as possible, this minimally invasive procedure aims to release pressure on the affected nerve root.
- Laminectomy: In a laminectomy, the lamina (a portion of the vertebra) is removed to make more room for the compressed nerves. When disc herniation and significant spinal stenosis coexist, this procedure is typically used.
- Spinal Fusion: Patients with persistent disc herniation or severe instability may want to consider spinal fusion. To stabilize the spine, it entails fusing two or more vertebrae together using bone grafts or implants.
- Artificial Disc Replacement: In a few circumstances, a damaged disc can be replaced with an artificial one, keeping the spine mobile and functional. Younger, more active patients frequently consider this option.
Precautions for Lumbar Disk Disease
For the spine to remain healthy and pain-free, lumbar disc disease prevention is crucial. Here are some essential tactics to aid you in preventing this condition:
- Maintain a Healthy Weight: Being overweight increases the strain on your spine and the likelihood of disc herniation. To reach and keep a healthy weight, practice regular exercise, and eat a balanced diet.
- Practice Good Posture: When standing, sitting, or lifting objects, keep your posture upright. Avoid hunching over or slouching as this can put too much strain on your spinal discs.
- Right lifting: The right way to lift something heavy is to bend at the knees and hips rather than the waist. While lifting, keep the item close to your body and avoid twisting.
- Regular Exercise: Exercise regularly to build stronger back and core muscles. Yoga, Pilates, and swimming are a few exercises that can increase flexibility and support your spine.
- Stretching: To keep your muscles and ligaments flexible, incorporate stretching exercises into your daily routine. Hamstrings, hip flexors, and lower back muscles should all be stretched.
- Keep Hydrated: Your spinal discs need to stay hydrated and healthy, so it's important to drink enough water. For your discs to continue to perform at their best, drink enough water each day.
- Quit Smoking: Smoking lowers blood flow to the spine, which can hinder damaged discs' ability to heal and raise the risk of degeneration.
- Healthy Diet: Eat foods high in calcium, vitamin D, and omega-3 fatty acids, as well as other nutrients that support the health of your bones and discs. If you have specific dietary worries, speak to a doctor or nutritionist.
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now









