Blood GroupBlood can be classified into distinct blood groups. These groups are formed on the basis of the presence or absence of certain antibody antigens. Both antibodies and antigens are found on the surface of the red blood cells. These compounds are hereditary. That is, they are transferred across generations. Using this statement, we can say blood group is not formed randomly in a child. It is formed due to the inheritance of particular compounds specifying a particular blood type. 
Antigens can be proteins, glycoproteins, lipids and carbohydrates, depending on the classification system. Some of these antigens can be found on the surface of numerous other cell types found in different organs. A blood group system comprises a number of these red blood cell surface antigens that can all come from the same allele (or different gene). An individual's blood type is inherited and reflects both parents' contributions. Due to the wide distribution of the type of antigens and antibodies, The International Society of Blood Transfusion has made at least forty-three different blood group systems for humans. Some examples are the usual ABO blood grouping or + or - a symbol for RhD blood status. Blood Grouping SystemsA person's blood type is one of several potential combinations of blood-group antigens; a full blood type would describe each of the 43 blood groups. The blood group present at the time of birth remains the same for the entire life. That is, blood groups, do not change with age or any other factor. However, there are a few exceptions where it can change. The main reason for the same is usually the addition or suppression of a particular antigen brought into the body through infection, autoimmune disorder or cancer. 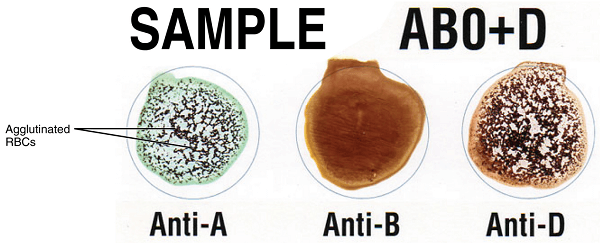
Another condition which can also change a person's blood type is a bone marrow transplant. Many leukaemia and lymphomas are treated through bone marrow transplants. When a person receives bone marrow from a donor who has a different ABO type than they do (for example, a type-A patient receiving a type O donor's bone marrow), the patient's blood type eventually changes to that of the donor. This is due to the fact that the patient's hematopoietic stem cells (HSCs) are eliminated either by bone marrow ablation or by the donor's T-cells. So, in such a scenario, the patient's original red blood cells will be completely replaced by new cells made from donor HSCs and patient's cells by that time will be perished. The new cells' surface antigens will differ from those on the surface of the patient's initial red blood cells, assuming the donor had a different ABO type. Some blood types are linked to the inheritance of certain disorders; the Kell antigen, for instance, is occasionally linked to McLeod syndrome. Blood types may influence an individual's susceptibility to infections; one example is the resistance to a particular variety of malaria exhibited in those missing the Duffy antigen. Population groups from regions with a high malaria prevalence had less of the Duffy antigen, perhaps due to natural selection. Blood Grouping System - ABOFour categories can be made based on the presence or absence of a specific antigen in a person's blood. When talking about the ABO type of blood grouping system, antigens and antibodies are considered. According to this classification, two types of antigen and two antibodies are present in human blood. They are antigen A and antigen B. The two antibodies are antibody A and antibody B. Red blood cells and serum antibodies both include antigens. 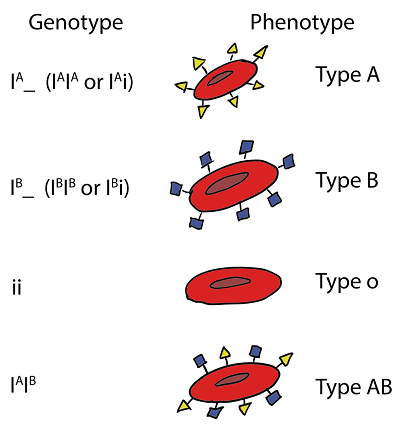
Along with the antigen, a specific pattern of antibodies is also present in human blood. The distribution of antibodies concerning antigens is as follows:
The relationship between antigen and antibody is due to their specific response toward each other. Such a response is called agglutination. It is seen that antigen A always agglutinates with antibody A. Similarly, antigen B agglutinates with antibody B. Moreover, blood transfusion is safe as long as the serum of the person receiving blood does not include antibodies to the donor's blood cell antigens. The most crucial blood-group system for transfusions of human blood is the ABO system. Immunoglobulin M, or IgM, are frequently linked to anti-A and anti-B antibodies. Although blood group compatibility guidelines are often applied to new-borns and infants, it has been postulated that ABO IgM antibodies are created in the early years of life by sensitization to environmental factors, including food, germs, and viruses. A/B/C was the initial nomenclature employed by Karl Landsteiner in 1901; "C" was eventually changed to "O" in later publications. Type O is frequently called 0 (zero or null) in other languages. Rh Blood GroupingWith 50 antigens today, this system ranks as the second-most important blood-group system in human blood transfusion. Of the five primary Rh antigens, the D antigen is the one that has the most potential to elicit an immunological response. It is typical for D-negative people to lack any anti-D IgG or IgM antibodies since sensitization to environmental factors trigger seldom results in the production of anti-D antibodies. However, after a sensitizing event, such as a blood transfusion containing D-positive RBCs or maybe a fetomaternal transfusion of blood from a pregnant woman, D-negative people might develop IgG anti-D antibodies. In certain situations, Rh's illness may manifest. Asian populations have a substantially lower prevalence of Rh-negative blood types (0.3%) than European cultures (15%). 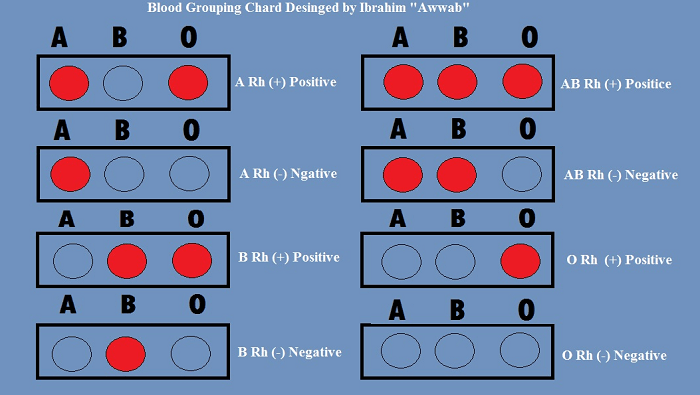
Other Blood Grouping StructuresAlong with the ABO and Rh systems, the International Society for Blood Transfusion has recognized 41 more blood-group systems as of 2021. As a result, the RBC surface membrane expresses several antigens in addition to ABO and Rh antigens. Numerous blood group systems bear the names of the patients who were first exposed to the appropriate antibodies. For instance, a person can have positive or negative blood group system antigens for AB, D, M, and N all at once (MNS system), K positive (Kell system), Lea or Leb negative (Lewis system), and so on. When combining blood from various persons, blood group systems other than ABO and Rh provide a potential but modest risk of problems. Clinical RelevanceBlood Donation The study of blood types and the activities of a blood bank to provide a transfusion service for blood and other blood products are topics covered by the specialist field of haematology known as transfusion medicine. Similar to how a licenced physician or surgeon must give drugs, blood products come under the same category. 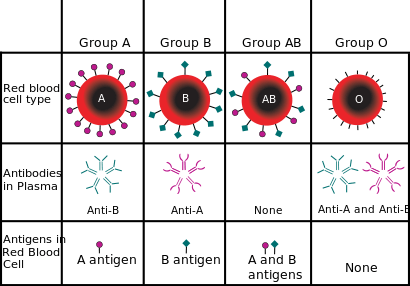
Blood from donors and receivers is tested routinely by blood banks to ensure that each recipient receives blood that is compatible with them and as safe as possible. If by any chance, during blood transfusion, incompatible blood is transfused in a person's body, it may risk his life. Various fatal risks are associated with incompatible blood transfusions like acute hemolytic response (destruction of RBCs), renal failure, and sometimes even death. To significantly hemolyze the transfused blood, highly active antibodies can assault RBCs and bind elements of the complement system. Blood transfusion is not an easy and risk-free process. Blood matching is done very accurately to avoid any fatal risk. It is always preferred that patients should be given either their blood or at least type-specific blood products during transfusion. Autologous blood transfusion is the type of blood transfusion where a person's blood is used for transfusion. It is always compatible with the person. Following are the steps for cleaning a patient's red blood cells:
Red blood cells can be washed in several ways. Centrifugation and filtration techniques are the two basic approaches. Microfiltration tools like the Hemoclear filter can be used for this technique. Cross-matching blood can further lessen risks; however, this step may be bypassed when blood is needed for an emergency. During the cross-matching of blood, the blood samples are taken from both the receiver and donor. The recipient's serum is mixed with the donor's red blood cells. It is then observed that clumps are not formed due to mixing. If clumps are formed, agglutination occurs, and blood is not matched. Blood bank technicians typically use a microscope to check for agglutination if it is not immediately apparent. Blood from that specific donor cannot be transfused to that specific recipient if agglutination occurs. All blood samples must be appropriately recognized in a blood bank. Hence labelling has been standardized using the ISBT 128 barcode system. Military members may wear identification tags or have tattoos with their blood group information on them in case they ever require an emergency blood transfusion. During World War II, the frontline warriors German Waffen-SS got blood type tattoos. 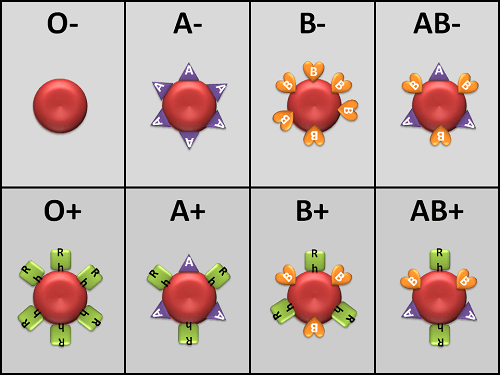
Hospitals and blood banks may have supply issues with rare blood types. For instance, Duffy-negative blood is more common in persons of African descent. The lack of Duffy-negative blood for these patients may be due to the blood type's rarity in the general population. Travelling to regions of the globe where supplies of RhD negative blood are scarce, notably East Asia, where blood services may try to persuade Westerners to donate blood, carries danger for RhD negative individuals. Newborn Hemolytic Disease (HDN)A pregnant woman might bear a child whose blood type differs from hers. Usually, if an Rh- woman gives birth to a kid with a Rh+ father and the child ends up being Rh+ like the father, this is a problem. The mother can produce IgG blood group antibodies in certain circumstances. For example, a tiny fetomaternal haemorrhage after birthing or obstetric intervention might cause some of the foetus' blood cells to enter the mother's blood circulation. This could also occur following a therapeutic blood transfusion. In the present and later pregnancies, this may result in Rh disease or another hemolytic disease of the newborn (HDN). This condition, known medically as hydrops fetalis, can occasionally be fatal for the foetus. Fetal DNA in maternal plasma can be analyzed to determine the fetus's Rh blood type if a pregnant woman is known to have anti-D antibodies. This can help determine the risk of Rh illness to the foetus. One of the greatest achievements in medicine throughout the 20th century was the development of an injectable drug called Rho(D) immune globulin, which prevented the development of Anti-D antibodies in D-negative mothers. Some blood group-related antibodies can induce severe HDN, whereas others can only cause moderate HDN or are not known to cause HDN.
Next TopicBlood Pressure
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share









