Muscular Dystrophy
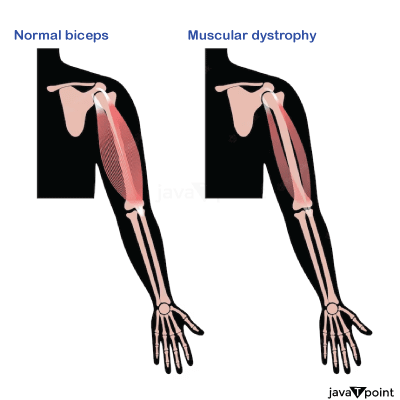
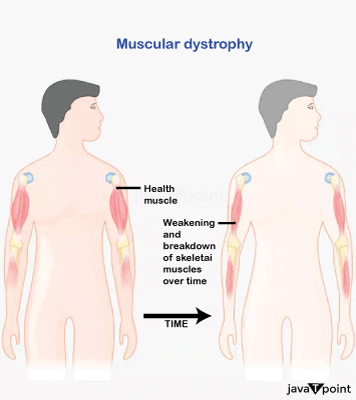
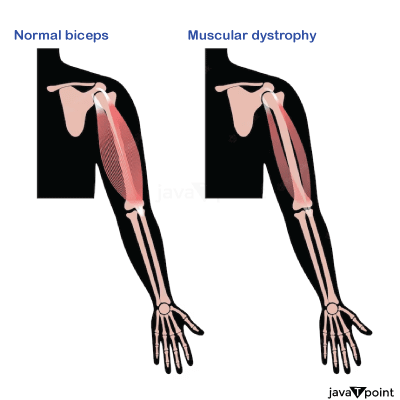
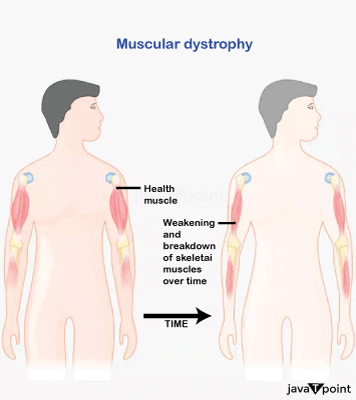
The term "muscular dystrophy" (MD) refers to a group of more than 30 genetic disorders that all have progressive muscle weakness and degeneration in common. Mutations in the genes in charge of regulating the structure and function of muscles are the main culprits behind these disorders. The fibres that make up muscles in the body contract and relax to allow for movement. These muscle fibres gradually degrade in people with muscular dystrophy and are replaced by fatty or fibrous tissue, which results in a loss of muscle mass and function.
Types
- Muscular dystrophy with Duchenne disease (DMD): DMD is one of the most prevalent and severe types of muscular dystrophy. The dystrophin gene, which is in charge of preserving the structure of muscle cells, has a mutation that causes it to primarily affect boys. Children with DMD typically begin to experience symptoms between the ages of 3 and 5, and the condition quickly worsens, impairing mobility and shortening lifespan.
- Becker Muscular Dystrophy (BMD): Though less severe than DMD, BMD is akin to it. A dystrophin gene mutation also causes it, but the symptoms show up later in childhood or adolescence, and the disease progresses more slowly. People who have BMD frequently have some degree of mobility throughout their lives.
- Myotonic Dystrophy: This kind of muscular dystrophy is characterised by myotonia, a condition in which muscles contract and then struggle to relax. Muscles, the heart, and the central nervous system can all be impacted by it, which is brought on by mutations in the DMPK gene.
- Limb-Girdle Muscular Dystrophy (LGMD): LGMD is the name for a group of diseases that primarily affect the muscles in the shoulders and hips. There are various subtypes of LGMD, and each is linked to particular genetic mutations.
- Facioscapulohumeral Muscular Dystrophy (FSHD): The muscles of the face, shoulders, and upper arms are particularly affected by FSHD. It typically manifests in adolescence or early adulthood and is brought on by a DUX4 gene mutation.
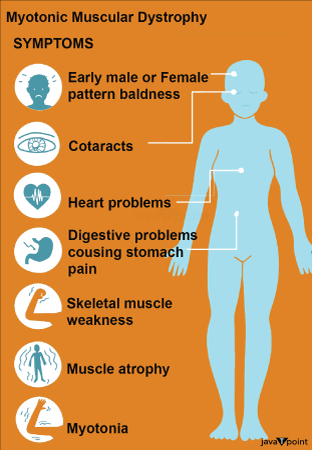
Symptoms
Depending on the specific type and severity of the disorder, muscular dystrophy symptoms can vary greatly. However, some widespread signs and symptoms include:
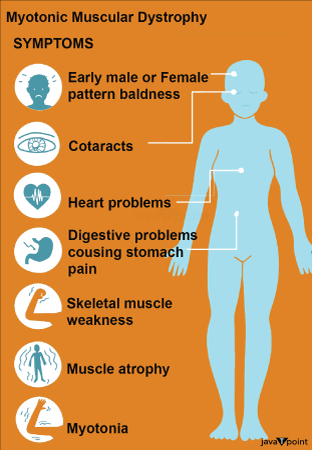
- Progressive muscle weakness: Weakness frequently starts in the body parts that are closest to the centre, like the hips and shoulders, and over time spreads to other muscle groups.
- Muscle wasting is the loss of muscle mass as a result of the replacement of degenerating muscles with fibrous or fatty tissue.
- Mobility restrictions: People who have muscular dystrophy may find it difficult to walk, climb stairs, or carry out basic daily tasks.
- Muscle cramps and stiffness: Some forms of muscular dystrophy are accompanied by muscle cramps and stiffness, especially after periods of inactivity.
- Muscular dystrophy can affect the breathing muscles, which can cause respiratory issues and, in severe cases, the need for assisted ventilation.
- Cardiomyopathy and other cardiac complications can be caused by specific types of muscular dystrophy that also affect the heart muscle.
Causes of Muscular Dystrophy
The following are some of the main causes and risk factors for muscular dystrophy:
- Genetic Mutations: Genetic mutations that affect the synthesis or functionality of essential muscle proteins are the main cause of muscular dystrophy. These mutations can occur in a number of different genes, each of which is linked to a specific type of muscular dystrophy. For instance, Duchenne and Becker muscular dystrophies are brought on by mutations in the dystrophin gene, whereas myotonic dystrophy and facioscapulohumeral muscular dystrophy are caused by mutations in the DMPK and DUX4 genes, respectively.
- X-linked recessive, autosomal dominant, and recessive autosomal patterns are all possible inheritance patterns for muscular dystrophies. A single mutated gene from a single parent is all that is necessary to cause the condition in autosomal dominant inheritance. Two copies of the mutated gene are passed down to the affected person through autosomal recessive inheritance, which requires both parents to carry the mutation. The mutation is carried on the X chromosome and is inherited in a recessive manner, affecting men more than women.
- Sporadic Mutations: Even in cases where there is no known family history of the condition, sporadic mutations can sometimes cause individuals to develop muscular dystrophy. The development of reproductive cells (eggs and sperm) or the early stages of embryonic development are two possible times when these mutations can occur.
- Genetic Variation: Different types of muscular dystrophy are caused by different gene mutations, which result in unique clinical characteristics and rates of progression. For instance, myotonic dystrophy is brought on by expanded repeats in the DMPK gene, whereas Duchenne muscular dystrophy is brought on by mutations that impair the function of the dystrophin gene.
- Genetic Testing: Genetic testing is frequently used to diagnose and pinpoint the specific genetic mutation that causes a person's muscular dystrophy. This makes it possible for a more precise diagnosis and can offer useful data for genetic counselling and family planning.
Laboratory Tests for Diagnosis
- Serum Creatine Kinase (CK) Levels: A preliminary blood test frequently includes determining the serum levels of CK. Due to the release of this enzyme into the bloodstream by damaged muscle cells, elevated CK levels are a frequent finding in many forms of muscular dystrophy. Elevated CK levels are not unique to muscular dystrophy, but they can offer a clue.
- Electromyography: A diagnostic procedure called electromyography (EMG) measures the electrical activity of the muscles. EMGs record electrical signals by inserting tiny needle electrodes into particular muscles. Identification of muscle damage or dysfunction can be aided by abnormal patterns of muscle activity.
- Nerve Conduction Studies (NCS): To assess how effectively the nerves transmit electrical signals to the muscles, NCS is frequently conducted in conjunction with EMG. This examination can aid in determining whether a condition is nerve- or muscle-related.
- Muscle Biopsy: A muscle biopsy may occasionally be required to confirm the diagnosis of muscular dystrophy. A biopsy involves surgically removing a small sample of muscle tissue to be examined under a microscope. This can show the degeneration of muscle fibres and the replacement of lean tissue that are hallmarks of muscular dystrophy.
Genetic Testing
- Genetic counselling: Genetic counselling is frequently advised prior to genetic testing. Genetic counsellors help people and families make well-informed decisions about testing by educating them on the advantages and restrictions of genetic testing, and addressing the implications for family members.
- DNA sequencing: It is typically used in genetic testing for muscular dystrophy to identify specific genes linked to the suspected type of the disease. For instance, dystrophin gene mutations have been linked to Duchenne and Becker muscular dystrophies. These mutations can be located and the diagnosis confirmed using molecular genetic testing.
- Multiplex Ligation-dependent Probe Amplification (MLPA) is a method for finding large deletions or duplications in the dystrophin gene, which may be the cause of some cases of Duchenne or Becker muscular dystrophy.
- Next-Generation Sequencing (NGS): NGS technologies have revolutionised genetic testing by enabling the simultaneous sequencing of numerous genes linked to different types of muscular dystrophy. When the precise subtype is unknown, NGS can offer a thorough analysis.
- Genetic Panel Testing: In some circumstances, a more comprehensive genetic panel may be used to examine a variety of neuromuscular genes, assisting in the identification of more uncommon types of muscular dystrophy or overlapping diseases.
- Whole Exome Sequencing (WES) or Whole Genome Sequencing (WGS): These cutting-edge genetic testing techniques can find gene mutations in any individual's exome (WES) or genome (WGS) by sequencing the entire exome or genome of the individual. When conventional genetic testing has failed to provide a diagnosis, these methods are helpful.
Treatment of the Disease
In order to maintain and enhance muscle function, mobility, and general quality of life, physical therapy is a crucial component of managing muscular dystrophy. Designing individualised exercise programmes and strategies to meet particular needs is a crucial responsibility for physical therapists. In physical therapy and rehabilitation for muscular dystrophy, important components include:
- Exercises that increase range of motion: Light stretches are important for maintaining joint flexibility and preventing contractures (tight muscles).
- Targeted resistance exercises for building strength can help slow muscle atrophy.
- Functional Mobility Training: Therapists focus on maximising mobility, using methods for secure gait, transfers, and posture.
- Respiratory muscle weakness is a common symptom of muscular dystrophy. Lung function can be preserved with the aid of breathing exercises and chest physical therapy.
- To increase independence and safety, therapists can evaluate and suggest assistive devices such as wheelchairs, braces, and orthotics.
Medications
Corticosteroids
Patients with MD are frequently given corticosteroids like prednisone and deflazacort.
They have been demonstrated to have the following advantages:
- Corticosteroids have an anti-inflammatory effect, which helps to lessen muscle tissue inflammation, a common symptom of many types of MD. They might aid in slowing the deterioration of muscles by reducing inflammation.
- Increased Muscle Strength: Some MD sufferers report increased muscle function and strength while taking corticosteroids. Mobility and general quality of life may both benefit from this.
- Delayed Disease Progression: According to studies, certain types of MD, such as Duchenne muscular dystrophy (DMD), may progress more slowly as a result of corticosteroids.
Cardiovascular Management Drugs
- Cardiac complications are a common complication of MD, especially in those with Duchenne muscular dystrophy. Medications to treat these side effects could consist of:
- Angiotensin-Converting Enzyme (ACE) Inhibitors: These drugs, such as enalapril and lisinopril, assist in controlling high blood pressure and lessen the burden on the heart. When MD patients develop cardiomyopathy (heart muscle disease), they may benefit from them.
- Beta-Blockers: For people with MD, beta-blockers like carvedilol and metoprolol can help control blood pressure and heart rate, lowering their risk of developing heart failure.
- Diuretics: If you have heart-related symptoms, your doctor may presrcibe a diuretic like furosemide to manage fluid retention and lessen swelling.
- Anti-Arrhythmic: In some circumstances, drugs that regulate abnormal heart rhythms (arrhythmias) may be required.
- These drugs are a crucial component of managing cardiac complications in MD and are typically presrcibed by a cardiologist.
Drugs for Pain Management
Due to joint problems, stiffness, and muscle weakness, people with MD may experience varying levels of pain. The following are some examples of painkillers:
- Non-steroidal anti-inflammatory drugs, or NSAIDs, such as ibuprofen and naproxen, can help relieve pain and lessen inflammation in muscles and joints. The potential side effects of NSAID use over an extended period of time call for monitoring.
- Muscle relaxants: Drugs such as baclofen or tizanidine may be presrcibed to treat muscle spasms and lessen the discomfort they cause.
- Painkillers: For severe pain that does not improve with other treatments, doctors may occasionally presrcibe opioids or other painkillers. Due to the possibility of dependence and side effects, their use is strictly regulated.
- Healthcare professionals should regularly evaluate the efficacy and safety of these medications and tailor pain management to the individual's unique needs.
Supplements to Diet
Muscular dystrophy management may involve nutritional supplements:
- A vitamin D deficiency may occur in people with limited mobility, so vitamin D supplements may be advised. For the health of your bones and general well-being, you need enough vitamin D.
- Calcium: Calcium supplements may be recommended, particularly when corticosteroids are being used, to support bone health and prevent osteoporosis.
- Coenzyme Q10 (CoQ10): Due to possible low levels of this antioxidant in people with MD, some of them take CoQ10 supplements. Muscle function may benefit from CoQ10, according to some research.
- Given that their overuse or misuse can have negative effects, supplements should only be used under the supervision of a healthcare professional.
Emerging and Experimenting Therapies
There has been a lot of investigation into new and experimental treatments for muscular dystrophy in recent years. Although not yet widely available, these treatments show promise. Here are a few instances:
- Gene therapy is a technique used to replace or correct the faulty genes that cause MD. Gene therapy strategies are being investigated in several clinical trials for various types of MD.
- Exon skipping: In people with specific types of MD, such as Duchenne muscular dystrophy, exon skipping is a method that may be able to restore the production of a functional protein.
- Stem Cell Therapy: Stem cell therapy research is currently being conducted with the aim of repairing damaged muscle tissue and improving muscular function.
Precautions To be Taken
Muscular Dystrophy sufferers should take the following precautions:
- Maintain scheduled medical appointments in order to track the condition's development and address any new problems as they arise.
- Fall Prevention: To make your surroundings safe, take out any potential tripping hazards, put up grab bars and use mobility aids as necessary.
- Balanced nutrition is important because people with MD are more prone to fractures. Maintaining a well-balanced diet will help your overall health and bone strength.
- Assistive Devices: To maintain independence and lower the risk of injury, use mobility aids and assistive devices as directed.
- Avoid Overexertion: Exercise at a level that is appropriate for your age and fitness level, and steer clear of activities that could strain or injure your muscles.
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now









