Gram-Negative BacteriaBacteria that do not retain the crystal violet stain employed in the Gram staining technique of bacterial identification are known as Gram-negative bacteria. They have a characteristic cell envelope which is made up of a thin peptidoglycan cell wall. This is around it by an inner cytoplasmic membrane and an outer bacterial cell wall. 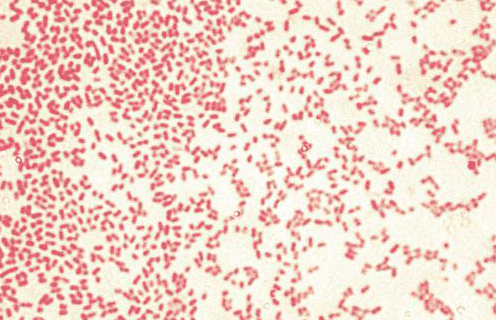
Due to their great resistance to medicines, Gram-negative bacteria (GNB) are one of the world's most serious public health issues. Since these germs often necessitate patients to remain in the intensive care unit (ICU), where they are at a high risk of morbidity and death, they are of major clinical relevance in hospitals. Most clinical isolates are caused by two broad groups: Enterobacteriaceae and non-fermenters; however, additional clinically relevant gram-negative organisms exist, such as Neisseria, Haemophilus spp., Helicobacter pylori, and Chlamydia trachomatis. Due to their great resistance to medicines, Gram-negative bacteria (GNB) are one of the world's most serious public health issues. Gram-Negative bacteria are very potent disease-causing organisms as they take patients to the Intensive Care Unit and cause a high rate of death and morbidity. Gram-negative bacteria may be found in almost every living area on the planet. Some of the important examples of gram-negative bacteria are Yersinia pestis, Pseudomonas aeruginosa, and Chlamydia trachomatis. They are resistant to so many medicines and antibiotics because of the presence of their tough outer membrane, which protects them not only from the medicines but also the detergents. These detergents would otherwise destroy the bacteria's inner cell membrane and affect the lysozyme. Lysozymes are antibacterial enzymes usually produced by animals as part of protection conferred by their immune system. Apart from this, even if the cell is able to kill these bacteria with the help of its immune system, the outer leaflet of the bacterial membrane contains a hazardous compound, lipopolysaccharide, whose lipid component is very dangerous for the cells. Low blood pressure, respiratory failure, decreased oxygen supply, and lactic acidosis are all symptoms of septic shock caused by its toxic response. 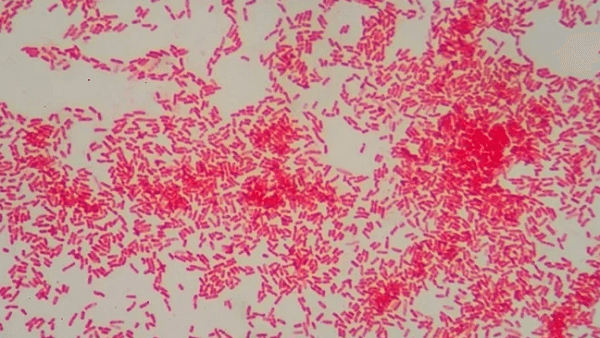
So many different kinds of antibiotics have been developed to kill Gram-Negative bacteria, for example, cephalosporins, Folate antagonists, piperacillin-tazobactam, ureidopenicillins, lactam-beta-lactamase inhibitor, carbapenems, and quinolones. They are specially developed to target specifically Gram-Negative bacteria, but sometimes they are also effective against some Gram-Positive Bacteria. CharacteristicsGram-negative bacteria (LPS-diderm) have the following characteristics:
ClassificationGram staining, like cell shape, is a quick diagnostic test that was originally used to categorize species in the Bacteria subdivision. Firmicutes (+), Gracillicutes (), Mollicutes (0), and Mendocutes (0) were formerly the four divisions of the kingdom Monera based on Gram staining (var.). Molecular research has been used to dispute the monophyly of gram-negative bacteria since 1987. However, some authors like Cavalier-Smith consider it a monophyletic taxon and refers to the group as the "Negibacteria" subkingdom. TaxonomyBacteria are generally divided into gram-positive and gram-negative bacteria based on their Gram-staining reaction. Bacteria are also divided on the basis of the number of membranes present in them. Gram-positive bacteria with one membrane are called monoderm, and gram-negative bacteria with two membranes are known as diderm bacteria. Traditionally, the groupings were assumed to represent lineages, with the additional membrane having only developed once, implying that gram-negative bacteria are more closely related to each other than gram-positive bacteria. While this is typically accurate, the categorization method fails in certain situations, producing lineage groups that do not match the staining result. As a result, Gram staining cannot be used to consistently determine bacterial family ties. Nonetheless, staining can frequently provide accurate information regarding the makeup of the cell membrane, such as the existence or absence of an outer lipid membrane. 
Monoderm prokaryotes are regarded to be the most primitive of the two structurally different kinds of prokaryotic organisms. The outer membrane of the Gram-Negative bacteria (diadems) is an adaptive advantage for their survival, as it protects them against antibiotic selection pressure. This theory is based on a number of observations, including some experiments where it is proved that Gram-Positive Bacteria are the most sensitive bacteria to antibiotics, whereas, the other hand, Gram-Negative bacteria are resistant. However, a class of bacteria exists, which is thought to represent an intermediate class between Gram-Negative and Gram-Positive Bacteria. While Gram staining shows the characteristic of Gram-Positive Bacteria owing to the presence of a thick layer of peptidoglycan, they also show the presence of an outer cell membrane which is the characteristic of Gram-Negative bacteria. Deinococcus is an example of this class. Simple diderms without lipopolysaccharide (LPS), archetypical diderm bacteria with lipopolysaccharide in the outer cell membrane, and diderm bacteria with mycolic acid in the outer cell membrane are the three types of diderm bacteria (e. g., Mycobacterium). A special class of bacteria is distinct from other Gram-Negative bacteria by a conserved cell structure. A variety of bacteria has been identified with this nature. Some of them are Fibrobacterota, Chlamydiota, Planctomycetota, Acidobacteriota, Aquificota, Chlorobiota, Pseudomonadota, Bacteroidota, "Cyanobacteria", Hydrobacteria Verrucomicrobiota, and Spirochaetota. These bacteria belong either to the phylum Bacillota (a monoderm group) or branches in its vicinity. They are marked with the absence of the GroEL signature. Various pieces of evidence point out that these bacteria constitute a monophyletic group. Some of them are the presence of CSI as a part of traditional lipopolysaccharide in all the sequence species of gram-negative, and another evidence is the presence of outer membrane, which is present in all the species, and none of them has lost it in the evolutionary process. There are some medicinally significant species of Gram-Negative bacteria, out of which four forms are important as they cause sexually transmitted diseases, meningitis, respiratory problems, etc. Example of these are Neisseria gonorrhoeae. Neisseria meningitidis, Neisseria meningitidis, Moraxella catarrhalis, Haemophilus influenzae. The other medicinally important Gram-Negative bacilli are known to cause respiratory problems, urinary problems, gastrointestinal problems, and other diseases. Example of these are Klebsiella pneumoniae, Legionella pneumophila, Pseudomonas aeruginosa, Escherichia coli, Proteus mirabilis, Enterobacter cloacae, Serratia marcescens, Proteus mirabilis, Serratia marcescens. Some of the bacteria are also known to be linked to hospital-acquired illnesses, and hence they cause diseases like bacteria ventilator-associated pneumonia and secondary meningitis. Bacteria have the ability to transfer genetic material through the horizontal gene transfer method, and one of the main processes under this category is Bacterial transformation. The exogenous genetic material is transferred from one bacterium to another in horizontal gene transfer. The other two methods of horizontal gene transfer used by bacteria are conjugation and transduction. In conjugation, the genetic material is transferred between two bacterial cells through direct contact between the two cells by forming a bridge. On the other hand, in transduction, genetic material is transferred from one bacterial cell to another through indirect contact, that is, the injection of exogenous DNA by bacteriophage virus into the host bacterium. The genetic material travels through the intermediary medium during transformation, and absorption is entirely reliant on the recipient bacteria. About 80 kinds of bacteria were known to be capable of transformation as of 2014, about equally split between gram-positive and gram-negative bacteria. However, the number may be an exaggeration since some of the findings are based on single studies. 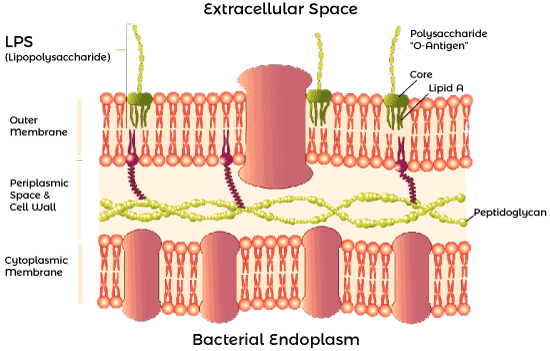
There are some bacteria which has been studied for transformation because they are medicinally important species. Some of them are Neisseria meningitidis, pylori, Haemophilus influenzae, Legionella pneumophila, Neisseria gonorrhoeae, and Vibrio cholerae. It's also been examined in gram-negative soil bacteria like Pseudomonas stutzeri and Acinetobacter baylyi, as well as gram-negative plant pathogens like Ralstonia solanacearum and Xylella fastidiosa. Disease RoleThe structure of gram-negative bacteria's outer membrane is one of its many distinguishing features. Lipopolysaccharide (LPS) is found on the membrane's outer leaflet, and its lipid A part serves as an endotoxin. If due, for some reason, Gram-Negative Bacteria is able to reach the circulatory system of animals, the lipopolysaccharide will activate the immune system, and an innate immune response will be triggered to produce cytokines a hormonal regulator. This causes inflammation and may lead to a toxic response, which can result in a fever, rapid breathing, and low blood pressure. This is the reason why Gram-Negative bacteria are known to cause life-threatening shocks. They're also resistant to detergent, dyes, and antibiotics, which are normally known to harm the bacteria. These bacteria are resistant to lysozyme and penicillin thanks to their outer membrane. It is because of the presence of an Outer wall that protects the inner membrane and the cell wall. Enzymes that break down or alter antibiotics are also found in the periplasmic space (the region between the two cell membranes). Treatments that are used to treat Gram-Negative infections include carboxy, Amino, and ureido penicillins. In order to fight against the enzymes that can digest these drugs, sometimes they are combined with beta-lactamase inhibitors. Beta-lactamase is an enzyme that is present in the periplasm. It is space, and it is known to digest these drugs. Examples of some of the medications given to treat the Gram-Negative infection include Cephalosporins, monobactams (aztreonam), aminoglycosides, quinolones, macrolides, chloramphenicol, folate antagonists, and carbapenems. Resistance to AntibioticsThese organisms inhibit many antimicrobials used in clinical treatment in a variety of ways. These include the methods to change the binding site of the drug, change in the conformational shape of the drug leading to deactivation of the resistance mechanism, and changes in membrane permeability. There are two membranes in GNB, one exterior and one inside. Lipopolysaccharide is considered a very strong immune response inducer, and it has three important components. These are a hydrophobic domain known as lipid A, hydrophilic polysaccharide, and antigen O. The hydrophobic domain is expressed on the outside of the cell membrane. It is the hydrophobic component lipid a, which is responsible for endotoxic actions. However, the LPS is variable across bacteria, and owing to genetic variations, some bacteria only produce a weak antigen that is not recognized by Toll-like receptors. There are, however, BGN groups that may elicit such a reaction in huge numbers. The immune system is also activated by some toll-like receptors 4 (TLR4), which are found in numerous cells involved in the immune system like macrophages, monocytes, neutrophils, and dendritic cells. The activation of the innate immune response mediated by LPS and TLR4 receptors results in an intensified response with the generation of cytokines, chemokines, and interferons, as well as inhibition of the response. The immune system's response is determined by the severity of the infectious process as well as the structure of the LPS in aggressive bacteria, which is linked to the virulence of the BGN. As a result, while some bacteria, such as E. coli, can induce the immune system, others, such as Helicobacter pylori, are only weakly antigenic. EnterobacteriaceaeThe Enterobacteriaceae family is a diverse collection of bacteria that may be found all over the world. They account for over 80% of gram-negative isolates in people, producing a variety of diseases such as urinary tract infections, pneumonia, diarrhea, meningitis, sepsis, endotoxic shock, and many more. Escherichia coli, Proteus, Enterobacter, Klebsiella, Citrobacter, Yersinia, Shigella, and Salmonella, are among the bacteria that often infect people. When it comes to microorganisms, laboratory characterization is critical. Therefore, it's critical to highlight the characteristics of Enterobacteriaceae, which are bacilli that are non-sporulated, have variable motility. Moreover, grow in the presence and absence of oxygen, ferment glucose-producing organisms, also are cytochrome oxidase negative, and can reduce nitrate to nitrite. Antimicrobial Resistance (Antimicrobial Resistance) (Antimicrobial Resistance) (Antimicrobial Resistance These organisms spread their plasmids by conjugation, resulting in resistance to practically all antibiotics now available. Given the potential for transmission across species and death rates owing to infections caused by bacteria carrying such plasmids, the carbapenemase family of enzymes - KPC, NDM-1, IMP, VIM, OXA-48 - is without a doubt one of the most serious health concerns of the century. Colistin, one of the few antibiotics still used to treat multiresistant infections, contains a mobile resistance gene, MCR-1, and Enterobacteriaceae has been implicated in the transmission of this gene, according to studies from throughout the globe. Furthermore, they often connect these genes with other resistance genes (CTX-M, NDM, IMP), resulting in resistance to cephalosporins and carbapenems, amplifying the germs' harmful effects. Non-FermentersWhen compared to Enterobacteriaceae, non-fermenter, gram-negative bacilli (BNF) have a lower incidence of isolation; yet, they are a significant category since they cause serious, deadly infections, particularly in hospitals. In ICU, patients undergoing invasive operations also trigger opportunistic illnesses. The most common BNF bacteria are Pseudomonas aeruginosa, Acinetobacter baumannii, Burkholderia cepacia, Stenotrophomonas, Alcaligenes, and Moraxella that cause illness in humans. These are notable for being aerobic and non-sporulated; they are unable to ferment carbohydrates and instead use them through the oxidative pathway. 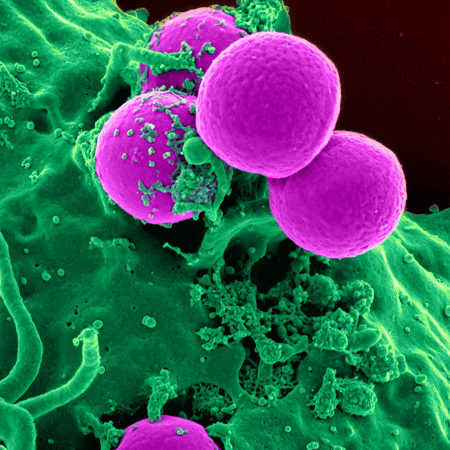
When it comes to antimicrobial sensitivity profiles, the most important problem with BNF is certainly their intrinsic resistance since they generate a range of genes with diverse pathways capable of dampening microbicidal effects. As a result, it distinguishes itself in P. aeruginosa, cephalosporins of type AmpC, and efflux systems that confer b-lactam resistance. The most common are MexAB-OprMand deletion of OprD (which causes bacterial cell impermeability owing to the lack of porin. Acinetobacter baumannii manufactures AmpC cephalosporins and oxacillinase (OXA) naturally, making it resistant to a variety of medicines. This microorganism's genetic cleverness goes even farther, combining great impermeability with genetic adaptability and resistance to mechanisms like extended-spectrum b-lactamases (ESBL). Stenotrophomonas have an innate multi-resistance pattern, particularly in individuals who have been exposed to carbapenems. Stenotrophomonas produces two carbapenemases, L1 (resistance to all carbapenems) and L2 (cephalosporins) and multiple efflux pumps. Whether they are linked or not, these processes severely limit therapeutic possibilities. Although it is susceptible to sulfamethoxazole-trimethoprim, it exhibits plasmid-mediated resistance. EtiologyGram-negative bacteria may infect practically every system in the human body, including the digestive system, neurological system, urinary system, and bloodstream, producing diarrheal gastroenteritis to serious meningitis. These germs invade the intestines, airways, and skin, making them more likely to spread to other regions of the human body, particularly in immunocompromised people. Furthermore, meningitis is a potentially lethal illness that may be acquired both in the community and in the hospital setting. Infections of the urinary tract are very prevalent, particularly in young women. However, with the widespread rise of multiresistant bacteria, these infections have become an issue. Finally, bacteremia is a serious consequence of these illnesses, owing to the microbes' resistance to antibiotics stated earlier. EpidemiologyAfter analyzing the ubiquitous nature of Gram-Negative bacteria and the potential with which it is harming humans and causing various infections, it is very critical to emphasize that the most important issue in the Healthcare world is to identify the bacterial groups that cause multi resistant illnesses. Due to the pathogens' poor response to antimicrobials, which the creation of ESBL and carbapenemases has essentially crushed, multi-resistant gram-negative infections (MDRs) are now one of the world's most serious health problems. The first KPC carbapenemase infection was recorded in the United States a little over two decades ago, and since then, similar infections have spread worldwide. However, since the 1980s, several reports have been reported of infections due to Gram-Negative esbl strain in hospitals infections caused by multi-resistance. Gram-Negative bacteria are very frequent in the United States, leaving only a few places like Maine and Idaho, according to the Centers for Disease Control and Prevention (CDC). Still, Livorsi et al. discovered a range of incidences in the United States, ranging from 0.3 to 2.93 illnesses per 100000 person-years. Multiresistant bacteria have previously been reported on practically every continent outside of the United States. Multidrug-resistant (MDR) diseases kill around 25000 persons in Europe each year. CTX-M, TEM, SHV, PER, VEB, and TLA) are extended-spectrum beta-lactamases that hydrolyze extended-spectrum cephalosporins. CTX-M and its variants are the most common enzymes in this class. They had linkages to the hospital setting at the start of the ESBL outbreaks, but now they're detected in patients who came from the community. Carbapenemases (KPC, NDM-1, IMP, VIM, OXA-48) are enzymes that hydrolyze carbapenems and other beta-lactam antibiotics. KPC, NDM, and OXA-48 are the most usually found in the United States; in Europe, OXA-48, KPC, and VIM are the most common, with NDM being less common. Furthermore, the transfer of these enzymes through plasmids, which often include additional resistance genes, makes these gram-negative bacteria pan-resistant. Finally, the great potential of interspecies transmission is another route for the worldwide dissemination of these genes. Patients with comorbidities, hospitalizations in intensive care units, past antibiotic usage, and continuous use of a central venous catheter are also thought to be at risk of getting a multidrug-resistant infection. Physical and historical contextGram-negative infections have non-specific symptoms that make it difficult to identify them from other infectious disorders on physical examination. Fever, chest discomfort, dyspnea, and purulent expectoration are common symptoms of pneumonia, which may be accompanied by tachycardia, tachypnea, hypoxemia, and auscultatory evidence of consolidation. These symptoms, however, are not unique to the condition. Cultures are the only method to figure out what creature you're dealing with. Some of the common symptoms of bacterial meningitis are prostration, severe headache, vomiting, mental disorientation, fever, neck stiffness, and nausea. However, such characteristics are not exclusive, and concluding, this kind of organism needs more data. 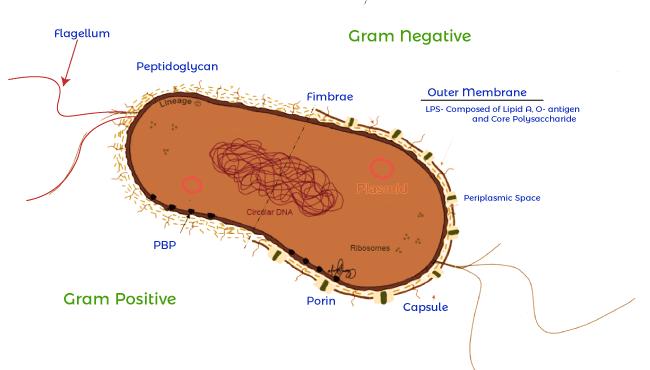
EvaluationWhile gram-negative infections are almost indistinguishable from infections caused by other etiologies, laboratory characterization may help identify the organism and its antibiotic susceptibility profile. The Gram stain is another important test for bacterial isolates; while basic, it may immediately discern the course of a therapeutic intervention. Enterobacteria are highly heterogeneous, and they can be identified by various biochemical tests like urease, catalase, cytochrome oxidase, motility citrate, DNAase, carboxylation of lysine, indole, and so on. These are cultured in primary isolation agar. Since E. coli is a powerful acid fermenter, it produces significant amounts of mixed acids, which raises the pH of the medium, resulting in pink colonies. As a consequence, cultures constitute the gold-standard evaluation of these illnesses, yet, they have the drawback of a long turnaround time. It is crucial to note, however, that identifying bacterial strains resistant to several medications may need the use of molecular technologies, which are not always accessible in labs. Phenotypic techniques that utilize EDTA like modified Hodge and combined diffusion disc are good alternatives. The MHT is a test that uses bacterial strains with carbapenemase enzymes to inactivate carbapenems, allowing a sensitive strain to grow to a disc carrying the antibiotic along the inoculum of the strain examined. This test is mainly advised for the strains with minimum inhibitory concentration or having a decreased zone of inhibition in the disc. Carbapenem antibiotic test disc is present in CDT consists of diffusion, in which carbapenem discs are inserted with and without EDTA, and their connection predicts whether the organism generates or does not make carbapenemase. Management / TreatmentThere are few treatment options for gram-negative MDR infections, and the outcomes are often dismal due to medication resistance. MDRs continue to evolve, resulting in resistance to new antimicrobials. As new medications become available, certain previously abandoned choices, such as polymyxins and colistin, which have considerable toxicity, have resurfaced (nephrotoxicity and neurotoxicity). Furthermore, medication resistance genes, such as MCR-1, have been discovered, raising further concerns. However, it is known that combining these medicines with carbapenems may boost their synergistic effect. Tigecycline is another option since it has shown in vitro efficacy against MDR; nevertheless, it has drawbacks, such as the need for large dosages and low tissue penetration, which limits its effectiveness in vivo. Fosfomycin, a once-common antibiotic used to treat urinary tract infections, has emerged as a possible treatment for MDR infections. However, monotherapy with this medicine leads to resistance. Thus, it's best used in combination with other antibiotics like carbapenems and polymyxin. These medicines can treat only tract infections because of their moderate absorption.. Aminoglycosides, formerly rejected because of nephrotoxicity and ototoxicity, have returned due to their potency against gram-negative bacteria. Except for urinary tract infections, these medications don't work as well against MDRs; they're also less toxic than polymyxin and tigecycline, so they might be effective in combination treatment. Differential Diagnosis is a term used to describe the process of distinguishing between two
Management of Toxicity and Side EffectsPolymyxins have been out of usage since the 1970s due to their well-documented toxicity, particularly their nephrotoxic effects. They resurrected after the introduction of gram-negative MDR pathogens. However, there have been instances of toxicity issues and increasing tolerance to certain medications. These medicines cause kidney damage primarily via oxidative stress, which results in mitochondrial malfunction and loss of this organelle's membrane potential. Another impact of this medication, which activates caspases 3, 8, and 9 in pulmonary epithelial cells, is apoptosis. The toxicity of polymyxins is proportional to their concentration. However, current pharmacokinetics and pharmacodynamics have already shown that the dose for this class of medications is insufficient, necessitating further research to address the problem, which might reduce the drug's toxicity. Aminoglycosides, which mostly induce ototoxicity and nephrotoxicity, are another family of medications having hazardous potential. These medicines are also responsible for the blockage of the cationic channels in the ciliated cells of the inner ear. They have the same effect on these cells' mechanosensitive transduction channels, causing metabolic changes that lead to an increase in intracellular calcium and the generation of reactive oxygen species (EROS), both of which cause irreversible cell death. The method by which these medications exert their toxicity is endocytosis, which results in the release of the lysosome's contents; also, they block calcium channels, resulting in the loss of this ion, as well as magnesium and potassium. PrognosisSince gram-negative infections have so many factors, determining the prognosis of illnesses caused by these bacteria is challenging and contradictory in the literature. However, such infections are frequently linked with a bad prognosis, especially in older patients, those with comorbidities, those who have had a solid organ transplant, and those who have malignant illnesses. The causative microorganism and infection location also determine treatment effectiveness. Serious infections with high death rates are linked to delayed or insufficient antibiotic treatment, while proper antibiotic delivery is linked to patient survival. Furthermore, the absence of a well-defined procedure for these infections may result in treatment failure due to inefficient or insufficient dosing, which leads to poor outcomes. Finally, monotherapy is inefficient, particularly when contrasted with combination treatment, associated with a favorable prognosis. ComplicationsMultidrug-resistant bacteria are becoming more common in the population, and such infections, if not treated effectively, may lead to renal failure, sepsis, and even death. Gram-negative infections, particularly enzyme makers that hydrolyze carbapenems, may cause a variety of problems. One of them is the urinary tract infection, becoming a worrying illness. Similarly, nosocomial infections in fragile patients with weakened immunity, comorbidities, and transitory immunosuppression provide a problem for health care providers. In this regard, people who have had burns need extra attention because there are more entrance points for germs, infections. Also it may be potentially fatal and invasive in such patients, depending on the microbial load and pathogen itself. Another concern is respiratory tract infections, which are most often linked with mechanical ventilation and are caused by gram-negative bacteria, including Enterobacteriaceae and non-fermenters, and have a high potential for mortality. Patient Education and DissuasionThe major challenge in the treatment of Gram-Negative infection, which is highly resistant, is the excessive use of antibiotics in hospitals. As MDRs grew more prevalent, it became clear that abuse of these antimicrobials was one of the contributing factors that needed to be addressed immediately. To modify the habit of the public and health professionals, efforts aimed at changing the use of these medications, such as educational campaigns, as well as the battle against self-medication, such as drug consumption monitoring and registration in pharmacies, are required. 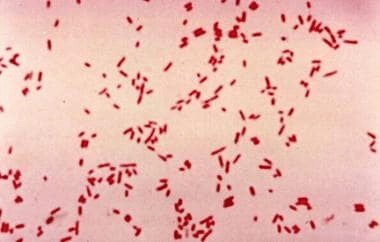
Improving the Performance of Healthcare TeamsThe infections caused by Gram-Negative bacteria, which are very resistant, are increasing at an alarming rate. However, eliminating drug-resistant pathogens is challenging due to a shortage of efficient medicines. As a result, basic precautions such as proper hand hygiene, disinfection of medical equipment, and isolation of patients suspected or diagnosed with MDR bacteria - particularly those undergoing invasive operations - with care about the admission of external individuals are recommended. Another important activity is for a laboratory worker who isolates MDR pathogens to quickly notify the epidemiological surveillance team at the health facility so that preventative and control measures may be implemented as soon as possible. Everyone should follow infectious disease prevention guidelines created in the healthcare system.
Next TopicAre bacteria Prokaryotes or Eukaryotes
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share









