Sexual Reproduction in HumansHumans reproduce sexually and are viviparous. Human reproduction processes comprise the formation of gametes (gametogenesis), i.e., male sperms and female ovum transfer of sperms into female reproductive tract (insemination) and the fusion of female and male gametes (fertilisation) that results in the creation of Zygote. This is followed by the formation and growth of the blastocyst, attaching it to the uterine walls (implantation), embryonic development (gestation), and the birth of the child (parturition). It is clear that these events of reproduction take place following puberty. There are significant distinctions between the events of reproduction for males and females. For instance, sperm production continues in men who are old. However, the ovum's formation ceases when women reach fifty years of age. Let's look at the female and male reproductive systems of the human. 
1. The Male Reproductive SystemA male's reproductive system is situated within the area of the pelvis. It comprises a pair of tests, along with glands, ducts, and the external male genitalia. 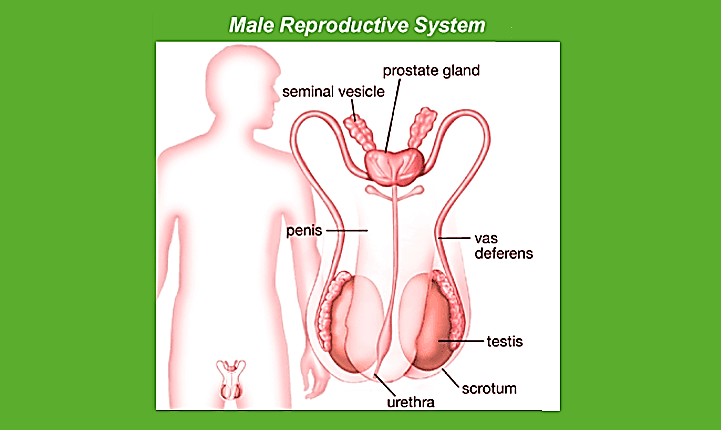
The testes are located inside the abdominal cavity in the pouch known as the scrotum. The scrotum assists in keeping the temperature of the testing areas (2-2.5 degrees Celsius lower than the average body temperature) vital to promote the process of spermatogenesis. For adults, the testis is oval and has a length of around 4 to 5 cm with a diameter of 2-3 cm. It is covered with a highly thick cover. Each testis contains about 250 compartments, referred to as the testicular lobules. Each lobule has up to three tightly curled seminiferous tubules where the sperms are created. Each seminiferous tube is lined with two kinds of cells known as male germ cells (spermatogonia) and Sertoli cells. The male germ cells undergo meiotic divisions, producing sperms as Sertoli cells provide nourishment to germ cells. The areas outside the seminiferous tubules are called interstitial spaces populated by small blood vessels, interstitial cells, and Leydig cells. Leydig cells produce and release testosterone from the testicle, known as androgens. Other immune-competent cells are also found. Male accessory ducts of sex comprise the epididymis, vasa-efferentia, and vas deferens. The seminiferous tubules that line the testis are opened to the vasa efferentia via the rete testis. The vasa efferentia depart from the testis and then open to the epididymis, located on the posterior portion of each testis. The epididymis is connected to the vas deferens, which then rise to the abdomen and loop around the bladder. It is connected to a duct by the seminal vesicle and then opens to the urethra via the ejaculatory canal. The ducts are used to store and transport the sperms out of the testis out through the urethra. The urethra is derived from the bladder of the urinary tract and extends from the penis to its exterior opening, which is known as the urethral meatus. The penis is the male's external Genital organ. It is composed of a particular type of tissue that aids in the erection of the penis and facilitates the process of insemination. The penis's larger end, called the glans penis covered by the skin's loose fold known as the foreskin. The male accessory glands consist of paired seminal vesicles, a prostate, and bulbourethral glands. The secretions from these glands comprise the seminal plasma, which is high in fructose calcium and certain enzymes. The secretions from the bulbourethral glands can also aid in the lubrication of the penis during coitus. 2. The Female Reproductive SystemFemale reproductive systems comprise of two ovaries as well as two oviducts, the uterus, vagina, cervix, and the external genitalia located in the pelvic area. The genitalia of these organs, together with mammary glands, are interconnected functionally and structurally to aid in ovulation, fertilisation, pregnancy, and the care of children. Ovaries are the primary female sex organs that create the gamete of a female (ovum) and a variety of hormones called steroids (ovarian hormones). Ovaries are situated on either side of the abdomen's lower part. Each ovary measures 2 to 4 centimeters in length. It is attached to pelvic walls as well as the uterus via ligaments. Every ovary is protected with a slim epithelium that covers the ovarian stroma. It is split into two zones: the peripheral cortex as well as the inner part of the medulla. 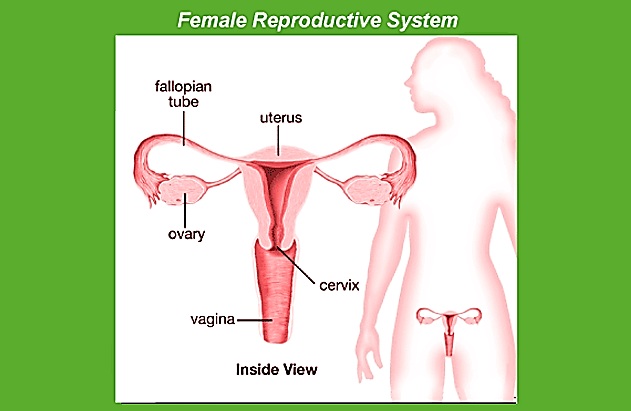
The female accessory ducts are formed by the oviducts (fallopian tubes), the uterus and vagina. Each fallopian tube is 10-12 centimeters long and extends from around the perimeter of the ovary until the uterus. The portion that is closer to the ovary forms the funnel-shaped infundibulum. The infundibulum's edges have finger-like projections known as fimbriae that assist in the collection of the ovum following the Ovulation. The infundibulum connects to a more significant portion of the oviduct, referred to as the ampulla. The final part of the oviduct isthmus has a small lumen that connects to the uterus. The uterus is a single organ, and it is also known as the womb. Its shape appears similar to an upside-down pear. The uterus is supported with ligaments bonded with the wall of the pelvis. The uterus expands into the vagina by an elongated cervix. The cervix's cavity is known as the cervical canal that, along with the vagina, form it into the birth canal. The uterus wall comprises three layers of tissues. The membranous exterior layer, the perimetrium, which is surrounded by a thick middle layer of smooth muscle myometrium and the glandular inner layer known as endometrium, which lines the uterus cavity. The endometrium goes through cycles of changes throughout the menstrual cycle, and the myometrium displays a significant contraction during the birth of the infant. The female external genitalia comprise the mons pubis and labia majora, hymen, and the clitoris. The mons pubis is a cushion made of fat tissue that is which is covered by pubic hair and skin. Its labia majora are tissues with fleshy folds extending downwards from the pubis mons and wrapping around an opening in the vaginal lining. Labia minora on the other hand are also paired folds made of tissue that are thin and are beneath the labia majora. The vagina's opening is typically covered in part by a membrane known as the hymen. The clitoris is a tiny finger-like structure situated at the upper intersection of two labia minora above the opening in the urethral canal. The hymen can be torn in initial coitus (intercourse). A functioning mammary gland is common to all female mammals. The mammary glands are pair structures (breasts) with glandular tissue as well as varying amounts of fat. The glandular tissue in each breast can be divided into 15 to 20 mammary lobes containing alveoli, clusters of cells. Alveoli cells produce milk stored within these spaces (lumens) found in the alveoli. Alveoli can open and expand into mammary tubes. The tubules in each lobe merge to make a mammary tube. Many mammary ducts join to form a mammary ampulla connected to a lactiferous duct, through which milk escapes. GametogenesisThe main organs of sex- the testis in males and the ovaries of females - make gametes, i.e., the ovum, sperms, for instance, through the process known as gametogenesis. In the testis, the male germ cells, which are not yet mature (spermatogonia), make sperms via spermatogenesis, which commences with puberty. It is believed that spermatogonia (sing. spermatogonium) are located on the inner seminiferous tubules' wall, multiplying through mitotic division and increasing. The spermatogonium itself is diploid and has 46 chromosomes. Certain spermatogonia are known as primate spermatocytes, frequently undergo meiosis. Primary spermatocytes go through the meiotic division (reduction division) that creates two haploid, equal cells, referred to as secondary cells called spermatocytes that have 23 chromosomes. Secondary spermatocytes undergo the second meiotic divide to make four identical, homozygous spermatids. They are transformed into spermatozoa (sperms) via a process known as spermiogenesis. After spermiogenesis is complete, the sperm heads are encased in Sertoli cells. Sertoli cells and then removed from seminiferous tubules through a process known as the spermiation process. Spermatogenesis begins at the age of puberty due to a significant increase in the release of gonadotropin-releasing hormone (GnRH). If you remember, this is a hypothalamic hormone. The elevated levels of GnRH will then act on the anterior pituitary gland and increase the secretion of two gonadotropins: the luteinising hormone (LH) and Follicle stimulation hormone (FSH). LH works on the Leydig cells, and it stimulates the production and secretion of androgens. Androgens, in turn, enhance the process of spermatogenesis. FSH is a stimulant for Sertoli cells and triggers the release of specific factors that aid in the process of spermiogenesis. Suppose we study the structure of the Sperm. It is a microscopic molecule comprised of the head, neck, a middle piece, and a tail. A plasma membrane surrounds the entire body of the sperm. The head of the sperm consists of an elongated haploid nucleus, a cap-like form, the acrosome, which encloses its anterior part. The acrosome is full of enzymes that aid in the fertilisation of the egg. The middle section is stuffed with mitochondria, which generate energy to move the tails that help sperm motility, vital for fertilisation. Human males ejaculate around 200-300 million sperms per coitus. For normal fertility, at least 60% of sperms should have a normal shape and size, in addition to at least 40%% of them having to show strong mobility. Sperms that come out of the seminiferous tubules get transported via these accessory ducts which are epididymis, vas deferens, seminal vesicle and prostate. Also these are essential for the motility and maturation of the sperms. The seminal plasma and the sperms make up the semen. The male glands and sex accessory ducts are maintained by testosterone hormones (androgens). The process of creating mature female gametes is known as Oogenesis that is distinct from the process of spermatogenesis. Oogenesis begins in the early stages of embryonic development when a few million gamete mother's cells (oogonia) are created in each ovary of the fetus; the oogonia does not form again and is then added after birth. They begin division and move into prophase I of meiotic division. They are temporarily halted at this stage, referred to as primary Oocytes. The primary oocytes are covered by a layer of granulosa cells and are referred to as the primary follicle. Many of these follicles become degenerate in the time from birth to puberty. So, when puberty occurs, there are only 60,000 to 80,000 primary follicles remaining in every ovary. The primary follicles are then enclosed by layers of granulosa cell layers and an additional theca. They are referred to as secondary follicles. The secondary follicle is soon transformed into a tertiary follicle that is distinguished by a fluid-filled cavity known as an Antrum. The theca layer can be divided into an inner theca internea and an external theca externa. It is vital to draw your attention to the fact that it's in this phase that the primary oocyte inside the tertiary follicle expands in size and is able to complete the primary meiotic divide. It is an unequal division that results in creating a huge secondary oocyte with haploids and a tiny polar body. The secondary Oocyte preserves the bulk of the abundant cytoplasm of the primary Oocyte that is rich in nutrient. As of now, we aren't entirely sure about this. The tertiary follicle then transforms into the maturing follicle known as Graafian follicle. The secondary oocyte creates an additional membrane known as zona pellucida that surrounds it. The Graafian folly then breaks and releases the secondary Oocyte (ovum) out of the ovary through a process known as ovulation. Fertilisation and ImplantationDuring coitus, semen is released by the penis and deposited into the vagina (insemination). The sperms that are motile swim quickly through the cervix before entering into the uterus and then reach the ampullary part in the fallopian tube. The ovum produced from the ovary is transferred to the ampullary region, where fertilisation occurs. Fertilisation only occurs when the sperm and ovum are simultaneously transported to the ampullary area. This is why not all copulations result in fertilisation and conception. A process for fusing the ovum with sperm is known as fertilisation. In the process of fertilisation, it is when sperm comes into proximity to the zona pellucida layer in the ovum. This causes changes to the membrane that stop the entry of other fertilised sperms. This ensures there is only one single sperm that can fertilise the ovum. The acrosome's secretions assist the sperm in entering the ovum cells by the zona pellucida and the plasma membrane. This triggers the conclusion of meiotic division in the secondary oocyte. The meiotic division that follows is not equal and leads to the formation of a second polar body and an ovum that is haploid (ootid). Soon, the haploid nucleus of the sperms and the ovum join to create an ovum that is a diploid Zygote. As you are aware, the chromosome pattern of the female of the human race is XX, while that of the male is called XY. So, all gametes that are haploid (ova) created by females are XY. Male sex chromosome, while for male gametes (sperms), the sex chromosome can be either X or Y. Therefore, 50% of sperms have the X chromosome. In comparison, the remaining 50% have the Y. After the fusion of gametes of females and males, the zygote could be XX or XY dependent on whether the sperm carrying either X or Y fertilised the egg. The zygote having XX could grow into a female infant, and XY will develop into a male. The mitotic division occurs as the zygote is moved through the oviduct's isthmus called cleavage to the uterus and then forms 2, 4, 8, 16 blastomeres, which are daughter cells. The embryo has eight to 16 blastomeres known as morula. The morula divides and changes into blastocysts as it grows further towards the uterus. The blastomeres of the blastocyst form an outer layer known as trophoblast and an inner layer of cells attached to the trophoblast, referred to as an inner cell mass. The trophoblast layer is connected to the endometrium. The inner cell mass is transformed into an embryo. After attachment, the uterine cells divide quickly and cover the blastocyst. This is why the blastocyst gets encased within the uterus' endometrium. This is known as the process of implantation and can lead to the birth of a baby. Pregnancy and Embryonic DevelopmentFollowing the implantation, finger-like projections develop on the trophoblast known as the chorionic villi, which are covered by uterine tissue and maternal blood. The uterine villi and the chorionic tissue join together and constitute a functional and structural unit that connects the embryo (foetus) and the mother's body, known as the placenta. The placenta assists in the delivery of oxygen, nutrients, and other substances to embryos and the elimination of carbon dioxide and excretory waste material generated in the embryo. The placenta is linked to the embryo via an umbilical cord that aids in the transportation of various substances from and to the embryo. The placenta is also an endocrine organ and produces multiple hormones, including human gonadotropin (hCG) and human placental Lactogen (hPL) hormones, estrogens progestogens etc. In the final stage of the pregnancy process, a hormone known as relaxin is also released through the ovary. We must be aware that hCG, relaxin, and hPL are made by women during pregnancy only. Additionally, during pregnancy, hormone levels such as estrogens, progestogens, cortisol, prolactin, and thyroxine etc. increases. These hormones are increased by many times in the maternal blood. The increased production of these hormones is crucial for helping to support the growth of the foetus, hormonal modifications in mothers, and maintaining the pregnancy. After the implantation, the tissue (embryo) transforms to form an outer layer called ectoderm and an inside layer, known as the endoderm. A mesoderm is soon visible between the ectoderm as well as the endoderm. These three layers are the ones that give birth to the entire tissue (organs) in adults. In this article, it is essential to note that the inner cell mass has specific stem cells, which can produce all organs and tissues. Human pregnancy is nine months. Human beings are the only mammals that can reproduce. After one month of gestation, the embryo's heart has been created. The first indication of a growing foetus can be observed by hearing the heart's sound with a Stethoscope. At the end of the 2nd month, the foetus is developing limbs and fingers. When the foetus is twelve weeks (first trimester), all major organ systems have been developed. For example, the internal genital organs and limbs are developed. The foetus's initial movements and the appearance of head hair are typically noticed in the 5th month. When the foetus is around 24-weeks (end in the 2nd trimester), body will be covered in fine hair, the eyelids are separated, and eyelashes grow. After nine months of gestation, the foetus has fully developed and prepared for delivery. Parturition and LactationThe typical human pregnancy lasts about nine months. This is known as the gestation time. A rapid contraction of the uterus after the termination of pregnancy results in the expulsion or delivery to the foetus. This procedure of delivery of embryos (childbirth) is known as parturition. A complex neuroendocrine system triggers parturition. Signals for parturition are derived from the fully developed foetus and placenta that trigger moderate uterine contractions known as foetal ejection reflex. This causes the release of oxytocin from the pituitary gland of the mother. Oxytocin affects the uterine muscle, causing more significant uterine contractions. This triggers the subsequent production of the hormone oxytocin. The reflex of stimulation between contraction of the uterus and the secretion of oxytocin continues to produce more and stronger contractions. This results in removing the infant from the uterus via the birth canal. This is known as parturition. After the baby is born, the placenta is eliminated from the uterus. The mammary glands develop during pregnancy and begin producing milk towards the end of pregnancy through the process known as lactation. This aids the mother to feed the infant. The milk produced during the first couple of days after lactation is known as colostrum that contains a variety of antibodies essential to building resistance for new-born infants. The practice of breastfeeding during the first few days of development of the infant is advised by medical professionals for the development of a healthy infant.
Next TopicLargest Cell in Human Body
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share









