Brain (Cerebral) EdemaIn the intracellular or extracellular spaces of the brain, there is an excessive buildup of fluid, referred to as cerebral edema. As a result, nerve activity is often hampered, the pressure within the skull is raised, and ultimately, the brain's tissue and blood arteries may be directly compressed. In general, symptoms include headaches, nausea, vomiting, seizures, sleepiness, visual problems, disorientation, and, in extreme instances, death. However, symptoms vary according to the location and degree of edema. In addition to ischemic stroke, subarachnoid haemorrhage, traumatic brain injury, subdural, epidural, or intracerebral hematoma, hydrocephalus, brain cancer, brain infections, low blood salt levels, high altitude, and acute liver failure, cerebral edema is often seen in a variety of brain traumas. The diagnosis is based on the physical exam results and symptoms, and serial neuroimaging (such as computed tomography and magnetic resonance imaging) is used to confirm it. 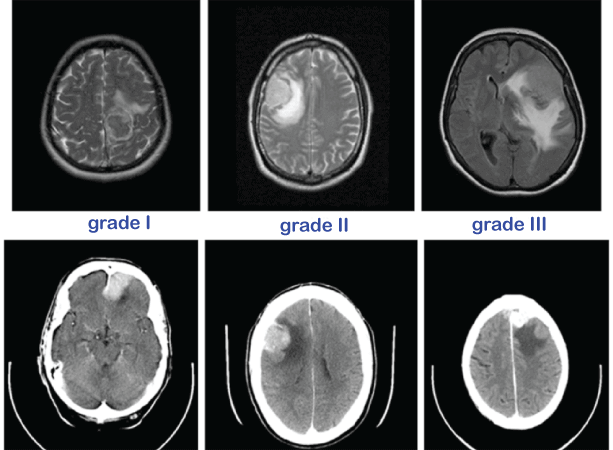
Depending on the underlying reason, cerebral edema may be treated with drugs, fluid management, steroids, correct posture, controlled hyperventilation, and monitoring of the patient's airway and intracranial pressure. A decompressive craniectomy is another surgical option for treating severe cerebral edema. A significant factor in the mortality of ischemic strokes and traumatic brain injuries, cerebral edema is one of the main causes of brain damage. The epidemiology of the illness is difficult to characterise since cerebral edema coexists with several prevalent brain diseases. The prevalence of this disease, which is present in the majority of instances of traumatic brain injury, central nervous system tumours, brain ischemia, and intracerebral haemorrhage, should be taken into account in terms of its probable causes. For instance, within 30 days following the commencement of an ischemic stroke, 31% of patients had malignant brain edema. Classification of Brain EdemaTraditionally, cerebral edema has been divided into two main subtypes: cytotoxic cerebral edema and vasogenic cerebral edema. This straightforward categorisation aids in diagnosing and managing individuals with cerebral edema. However, there are a number of additional distinct forms, such as interstitial, osmotic, hydrostatic, and high altitude-related edema, among others. Affected individuals might have many distinct subtypes present at once. 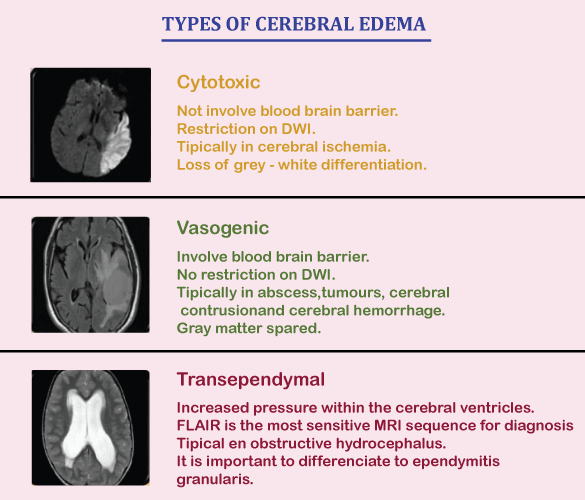
Individual sub-types of the following have been identified: 1. CytotoxicGenerally speaking, cytotoxic edema is connected to brain cell death by excessive cellular swelling. For instance, the blood-brain barrier is unaffected by cerebral ischemia. Still, the reduced blood flow and glucose supply cause disruptions in cellular metabolism and the production of energy molecules like adenosine triphosphate (ATP). The sodium and potassium pump in the cell membrane is impaired by the depletion of energy sources, which causes cellular retention of sodium ions. A buildup of sodium in the cell prompts a quick osmosis water absorption, which results in the cell's enlargement. The oncotic death of neurons is the ultimate result of cytotoxic edema. Cytotoxic edema is characterised by swelling of the individual brain cells, as opposed to vasogenic edema, in which the inflow of fluid is often seen in the interstitial space rather than inside the cells themselves. Given the different swelling and absence of a consistent "toxic" component, researchers have suggested that "cellular edema" may be a better word than "cytotoxic edema." Cytotoxic edema may be seen in a number of clinical situations, including: 2. VasogenicVasogenic edema, also known as extracellular brain edema, is brought on by an increase in blood-brain barrier permeability. Adhesion proteins bind the astrocytes and pericytes that make up the blood-brain barrier to form tight junctions. After an ischemic stroke, when blood flow returns to these cells, it may lead to excitotoxicity, oxidative stress, malfunction of the endothelial cells, and disruption of the blood-brain barrier. Fluid, ions, and plasma proteins like albumin extravasate into the brain parenchyma as a result of the blood-brain barrier's tight endothelial connections breaking down. The symptoms of cerebral edema are brought on by an extracellular fluid buildup that raises brain volume and, subsequently, intracranial pressure. Vasogenic edema may be present in the following clinical conditions: 3. Ionic (Osmotic)In ionic edema, the brain's osmolality (concentration of solutes) is higher than that of the blood, and the abnormal pressure gradient causes a buildup of water to enter the brain parenchyma by osmosis. The intact blood-brain barrier preserves the osmotic gradient. Several methods may dilute the blood plasma's solute concentration:
Due to a local plasma osmolality pressure gradient in comparison to the high osmolality in the damaged tissue, ionic brain edema may also develop at the sites of brain haemorrhages, infarcts, or contusions. 4. Interstitial (Fluid-filled)When there is a barrier to the cerebrospinal fluid's ability to exit the ventricular system due to noncommunicating hydrocephalus, interstitial edema is most easily identified. As a result of the blockage, the intraventricular pressure increases, and CSF leaks through the ventricle wall into the brain's extracellular fluid. The fluid's chemical makeup is similar to that of CSF. In addition to communicative hydrocephalus and normal pressure hydrocephalus, there are other causes of interstitial edema. 5. HydrostaticSevere arterial hypertension is often the cause of hydrostatic extracellular brain edema. Ultrafiltration of water, ions, and low molecular weight compounds (such as glucose and tiny amino acids) into the brain parenchyma is made possible by a difference in the hydrostatic pressure inside the artery system compared to the endothelial cells. The blood-brain barrier is often unbroken, and the arterial pressure determines how much edema is present. Up to systolic arterial pressures of 150 mm Hg, the regulatory mechanisms governing brain circulation may perform normally. At greater blood pressure, these mechanisms will work less effectively. Signs and Symptoms of Brain EdemaThe particular cause of cerebral edema will determine the amount and severity of the symptoms, although an abrupt rise in pressure within the skull often causes them. The Monro-Kellie concept states that since the skull is a permanent and inelastic structure, the buildup of cerebral edema may shift and compress essential brain tissue, cerebral spinal fluid, and blood vessels. A life-threatening surgical emergency, increased intracranial pressure (ICP) is characterised by headache, nausea, vomiting, and drowsiness. Visual abnormalities, including decreased vision, dizziness, and gaze paresis, are usually present in conjunction with symptoms. The Cushing reflex, characterised by erratic breathing and a slowed heart rate, may result from elevated blood pressure due to increased pressures within the skull, compensating for these pressures by raising blood pressure to maintain cerebral blood flow. The Cushing reflex often signals pressure on brain tissue and blood arteries, which reduces blood supply to the brain and ultimately results in death. Causes of Brain EdemaThere is a high prevalence of cerebral edema in acute brain injuries resulting from a number of causes, including but not limited to:
Risk factorsNumerous frequent brain diseases may produce cerebral edema, and the aetiology will determine the risk factors for its development. The following strokes have reliable indicators of early cerebral edema development:
Diagnosis of Brain EdemaSeveral neurological injuries often include cerebral edema. Therefore, it may be difficult to pinpoint the precise role that cerebral edema plays in the afflicted person's neurological condition. It is crucial yet demanding to closely monitor a person's level of consciousness and knowledge of any new or deteriorating focal neurological impairments, necessitating periodic admission to the intensive care unit (ICU). Brain herniation, prolonged increasing intracranial pressure, and cerebral edema is warning signs of potentially fatal catastrophic neurological events that must be identified and treated immediately. Therefore, early identification and prompt treatment of cerebral edema may improve clinical outcomes and mortality or risk of death. Based on the following, cerebral edema may be diagnosed: 1. ImagingSerial neuroimaging (CT scans and magnetic resonance imaging) may help identify or rule out intracranial haemorrhage, substantial masses, acute hydrocephalus, or brain herniation, as well as reveal the kind of edema present and the extent of the afflicted region. The preferred imaging technique is a CT scan, which is rapid, easy to use, and low-risk. CT angiography (CTA), MRI, or digital subtraction angiography (DSA) may be required in certain circumstances since a CT scan may not be able to pinpoint the precise aetiology of cerebral edema. The ability of MRI to distinguish between cytotoxic and vasogenic edema may help inform treatment choices in the future. 2. Monitoring of Intracranial PressureA key idea in traumatic brain injury (TBI) is the regulation of intracranial pressure (ICP). In people with TBI who have lower Glasgow Coma Scale (GCS) scores, abnormal CT scans, or extra risk factors, including advanced age or high blood pressure, the Brain Trauma Foundation recommendations advise ICP monitoring. There are no such recommendations for ICP monitoring in other types of brain traumas, such as ischemic stroke, intracerebral haemorrhage, and cerebral tumour. Based on clinical and radiological aspects, clinical studies have advised ICP and cerebral perfusion pressure (CPP) monitoring in any cerebrally injured individuals who are at risk of increased intracranial pressure. Early monitoring may be utilised to inform medicinal and surgical choices and find brain herniations that could be fatal. On the threshold levels of ICP that indicated the need for intervention, there were, however, inconsistent findings. Medical choices should be made according to the diagnosis (such as subarachnoid haemorrhage, traumatic brain injury, or encephalitis). ICP elevation should be combined with clinical and neuroimaging data rather than as a stand-alone predictive sign. Treatment of Brain EdemaMinor episodes of brain enlargement brought on by conditions like mild altitude sickness or a mild concussion often go away in a matter of days. However, further therapy is often required afterwards. While the swelling is reduced and any underlying causes are addressed, the aim is to ensure that the brain gets enough blood and oxygen to be healthy. A mix of surgical and medicinal procedures may be necessary to address this. In most cases, prompt treatment leads to a more full and rapid recovery. Without it, some harm may still exist. Supportive treatment options for brain edema may combine any of the following: >
Next TopicDysarthria
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share









