Myasthenia GravisMyasthenia gravis is a chronic autoimmune neuromuscular disease that weakens your skeletal muscles (the muscles that connect to your bones and contract to allow you to move your arms, legs, and breathe). Myasthenia gravis is characterised by muscle weakness that worsens with exertion and improves with rest. 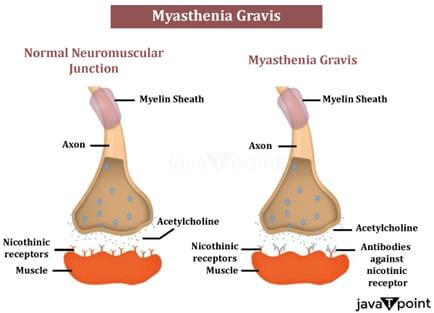
The disorder typically (though not always) involves specific muscles, such as:
Myasthenia gravis can strike without warning, and symptoms may not be noted right away. Individuals' levels of muscular weakness vary person to person. SymptomsMyasthenia gravis is usually associated with the following symptoms:
Myasthenia gravis can cause respiratory failure, which necessitates prompt emergency medical attention. Who is More Likely to Get Myasthenia Gravis?Myasthenia gravis affects both males and women, and people of all colours and ethnicities are affected. It primarily affects young adult females (under 40) and senior males (over 60), but anyone of any age, including children, can be affected. Myasthenia gravis is not hereditary or communicable. The disease might strike more than one member of the same family at times. Although infants are rarely affected by myasthenia gravis, the foetus may receive antibodies from a female parent, a condition known as neonatal myasthenia. Neonatal myasthenia gravis is usually transient, with symptoms disappearing within two to three months of delivery. Congenital myasthenia can occur in children born to healthy female parents. This is not an autoimmune illness, but it is caused by malfunctioning genes that produce aberrant proteins in the neuromuscular junction, which connects the end of a nerve that delivers information from the brain to a muscle and can cause symptoms similar to myasthenia gravis. Causes of Myasthenia Gravis
Neurotransmitters are molecules that allow neurons (brain cells) to communicate with one another. When an electrical impulse or signal travels through a motor nerve, the nerve ends release acetylcholine, a neurotransmitter that binds to acetylcholine receptors on the muscle. Acetylcholine connecting to its receptor stimulates and contracts the muscle. Antibodies (immune proteins produced by the body's immune system) block, modify, or destroy acetylcholine receptors at the neuromuscular junction in myasthenia gravis, preventing the muscle from contracting. Antibodies to the acetylcholine receptor are the most prevalent cause, but antibodies to other proteins, such as MuSK (Muscle-Specific Kinase), can also disrupt transmission at the neuromuscular junction.
How is Myasthenia Gravis Diagnosed and Treated?To confirm a diagnosis of myasthenia gravis, a clinician may perform or prescribe the following tests:
Because weakness is a typical sign of many other conditions, myasthenia gravis is frequently ignored or delayed (sometimes for up to two years) in people who have mild or localised weakness. Treating Myasthenia GravisThere is no known treatment currently. There are treatments available that help manage symptoms and allow you to live a normal life. Most people with myasthenia gravis live a normal life. Several treatments are available to assist reduce and improve muscle weakness, including:
Plasmapheresis is a machine-assisted technique for removing harmful antibodies from plasma and replacing them with healthy plasma or a plasma replacement. Intravenous immunoglobulin is a highly concentrated infusion of antibodies derived from a large number of healthy donors that temporarily alters the immune system's function. It acts by attaching to and eliminating the antibodies that cause myasthenia gravis from circulation. Some cases of myasthenia gravis may go into remission, either temporarily or permanently, and muscle weakness may totally subside, allowing medications to be stopped. What are the Latest Updates on Myasthenia Gravis?The National Institute of Neurological Disorders and Stroke (NINDS) is a division of the National Institutes of Health (NIH), the world's largest scientific research funder. Myasthenia gravis, its causes, and the anatomy and function of the neuromuscular junction are still being studied by researchers. Technological breakthroughs have resulted in more quick and accurate diagnosis of myasthenia gravis, as well as new and improved treatment choices. Researchers are attempting to create better pharmaceuticals, find new techniques to diagnose and treat people, and expand treatment options. MedicationSome persons with myasthenia gravis do not respond well to existing treatments, which often require long-term immune system suppression. New medications are being evaluated to see if they are more effective in addressing disease causes alone or in combination with existing therapeutic regimens. Biomarkers and DiagnosticsNINDS-funded researchers are investigating the formation and function of nerve-muscle fibre connections in order to better understand the underlying mechanisms in neuromuscular development, which could lead to new therapeutics for neuromuscular illnesses such as myasthenia gravis. Researchers are also looking into new ways to detect people with undetectable antibodies and identifying potential biomarkers (signs that can help diagnose or measure the progression of a disease) to predict an individual's response to immunosuppressive drugs. New Therapeutic OptionsA NINDS-funded study discovered strong data about the benefits of surgery for persons without thymoma, putting an end to a decades-long debate. Other trials will be conducted to see whether other medications are superior to standard care options. Assistive devices such as magnetic gadgets may benefit people. Better Care for Patients with Myasthenia GravisConsider taking part in a clinical study to help clinicians and researchers learn more about myasthenia gravis. Human trials are used in clinical research to assist researchers learn more about an illness and maybe identify better ways to diagnose, treat, or prevent disease. People of different ages, sexes, races, and ethnicities are needed, as well as those who are healthy or may have a problem or illness, to guarantee that study results apply to as many people as possible and that therapies are safe and effective for everyone who uses them.
Next TopicAphasia
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share









