Brain Surgery
Neurosurgery, also known as brain surgery, is a complex and specialised surgical field that focuses on the diagnosis, treatment, and management of a wide range of neurological disorders and conditions that affect the brain and nervous system. It includes a broad range of surgical techniques, each one designed to address a particular problem that may impair a person's cognitive, sensory, motor, or autonomic functions.
Conditions that require Brain Surgery
Some of the key conditions that may require brain surgery:
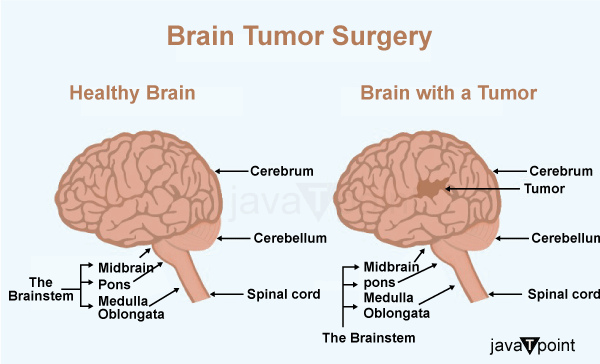
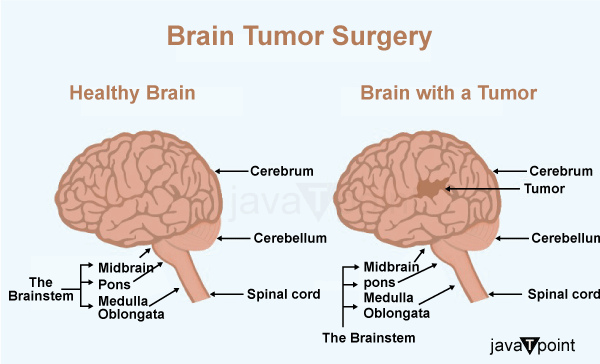
Brain Tumors: The presence of brain tumours is one of the most frequently cited justifications for brain surgery. Tumours can develop from various types of brain cells or from other cells that have migrated to the brain. They can be benign (non-cancerous) or malignant (cancerous). Tumours can put pressure on nearby brain tissue as they enlarge, leading to neurological deficits, seizures, headaches, and cognitive decline. The goal of surgery is to eliminate the tumour as much as possible while protecting healthy brain tissue. Before choosing an additional course of treatment, a biopsy may in some circumstances be carried out to ascertain the type of tumour.
Epilepsy: Surgery may be an option if medication for epilepsy is ineffective. The focus of the seizure can be eliminated in order to treat focal seizures, which start in a particular region of the brain.
Cerebrovascular Disorders: Surgery may be required for conditions like aneurysms and arteriovenous malformations (AVMs) that affect the blood vessels in the brain. Aneurysms are areas where the blood vessel walls are vulnerable to rupture, which can result in bleeding into the brain. AVMs are abnormal blood vessel tangles that can obstruct regular blood flow and cause bleeding. To stop haemorrhage and its potentially fatal consequences, surgery aims to treat aneurysms and eliminate AVMs.
Traumatic Brain Injury (TBI): Severe head injuries brought on by mishaps, slips, or other traumatic events can result in brain swelling, bleeding, or hematoma formation. Surgical intervention may be necessary to remove the blood, lower pressure, and stop further damage in situations where the pressure inside the skull rises to dangerously high levels.
Hydrocephalus: Increased intracranial pressure is caused by the buildup of extra cerebrospinal fluid in the brain's ventricles, which is a condition known as hydrocephalus. Placing a shunt system during surgery can effectively manage hydrocephalus and prevent brain damage by diverting extra fluid away from the brain and to another area of the body.
Stroke: Ischemic strokes are caused when a blood clot blocks an artery in the brain, reducing blood flow and possibly causing tissue death. To remove the clot and restore blood flow, surgical procedures like thrombectomy may be used in some circumstances. In order to relieve pressure and reduce damage in haemorrhagic strokes, which are brought on by bleeding in the brain, the hematoma may also need to be surgically removed.
Neurological Trauma: Fractures, tissue damage, or the presence of foreign objects inside the brain can result from severe head injuries or penetrating wounds. To fix fractures, remove debris, and treat any associated bleeding or swelling, surgery might be required.
Movement Disorders: Parkinson's disease, essential tremor, and dystonia are a few examples of movement disorders that can be extremely crippling. In order to manage symptoms and enhance the patient's quality of life, deep brain stimulation (DBS) surgery involves implanting electrodes into particular brain regions to modulate abnormal neural activity.
Pituitary Tumours: The pituitary gland, which is found at the base of the brain, is essential for the control of hormones. The hormonal balance can be upset by tumours in this region, which can result in a number of health problems. Surgery is frequently done through the nose (transsphenoidal approach), and its goals are to remove or reduce the tumour's size as well as to correct hormonal imbalances.
Chiari Malformation: The brainstem and cerebellum are displaced downward into the spinal canal as a result of the congenital condition known as Chiari malformation. To relieve pressure on the brainstem and re-establish regular cerebrospinal fluid flow, surgery might be required.
Trigeminal Neuralgia: Trigeminal neuralgia is characterised by excruciating facial pain and may be brought on by pressure on the trigeminal nerve. The goal of microvascular decompression surgery is to release this pressure, frequently by repositioning the blood vessels that are pressing on the nerve.
Abscesses and Infections: In order to stop an infection from spreading and causing more damage, infected tissue may need to be surgically removed as well as surgical drainage in cases of brain abscesses or encephalitis.
Functional Disorders: Brain surgery may be used in some cases to treat severe psychiatric or neuropsychiatric conditions, such as treatment-resistant depression or obsessive-compulsive disorder. To regulate brain activity and reduce symptoms, techniques like deep brain stimulation (DBS) may be taken into consideration.
Process of Brain Surgery
Getting Ready for the Operation:
- Medical Evaluation: Prior to brain surgery, patients go through a thorough medical evaluation that entails physical checks, imaging tests (like MRI or CT scans), and laboratory checks. The medical staff can better understand the patient's overall health and the specific condition that necessitates surgery thanks to this assessment.
- Neurological Assessment: A comprehensive neurological assessment is performed to gauge the patient's mental, motor, sensory, and cognitive abilities. This evaluation aids in creating a baseline for comparison during the healing process following surgery.
- Taking Consent: When a patient and their family or carers meet with a neurosurgeon to discuss a surgical procedure, the risks, advantages, and potential side effects are all covered. After confirming that the patient is aware of all the procedure's risks and potential benefits, informed consent is obtained.
- Pre-Operative Instructions: Patients are given detailed pre-operative instructions, such as requirements for fasting prior to surgery. Blood thinners and other medications that could conflict with the procedure may need to be temporarily stopped.
Surgical Procedure:
- Anaesthesia: The patient is taken to the operating room the day before the procedure and given anaesthesia to make sure they are unconscious and pain-free. The specific surgery being performed and the patient's health determine the type of anaesthesia to be administered.
- Craniotomy: A craniotomy is carried out during many brain operations. To access the brain tissue, a hole must be made in the skull. Depending on the surgical technique and the part of the brain being treated, the opening's size and location may change.
- Navigation and imaging: Surgeons may use sophisticated imaging methods to precisely locate the target area and direct them throughout the procedure, such as intraoperative MRI or computer-assisted navigation systems. Accuracy is improved, and the chance of harming healthy brain tissue is decreased.
- Tumor Resection or Intervention: Neurosurgeons carefully remove the abnormal tissue while preserving as much healthy tissue as possible if the goal of the surgery is to remove a brain tumour or lesion. Aneurysms and arteriovenous malformations are examples of vascular abnormalities, and the surgeon may choose to remove or repair the affected blood vessels.
- Electrophysiological Monitoring: In some circumstances, particularly when the surgery involves regions of the brain important for vital functions (like speech or movement), electrophysiological monitoring may be utilised to evaluate brain function in real-time and prevent harming functional areas.
Types of Brain Surgery
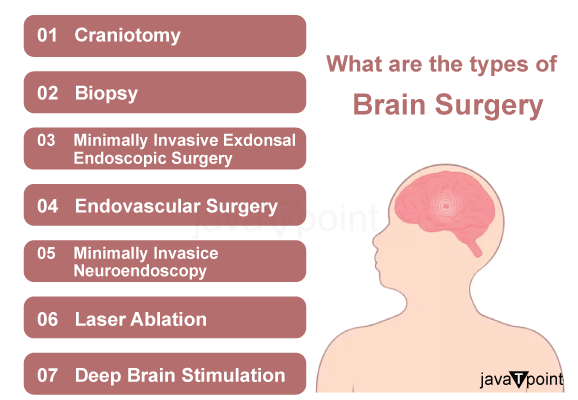
Some of the most common types of brain surgery and their applications are listed below:
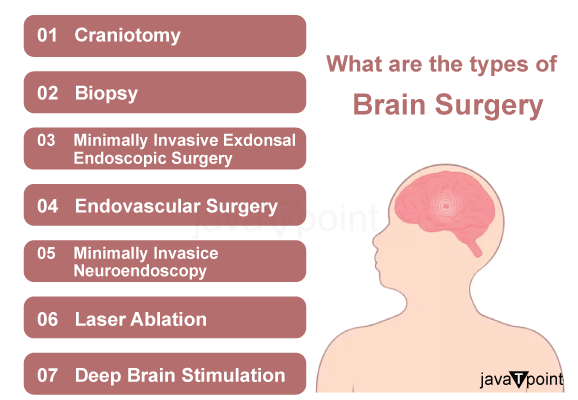
- Craniotomy: In order to access the brain, a basic neurosurgical procedure called craniotomy involves removing a portion of the skull. It is carried out for a variety of purposes, including the treatment of traumatic brain injuries, the removal of tumours, the treatment of brain aneurysms, and hematoma evacuation (the removal of blood clots). Once the procedure is finished, the bone flap that was removed is typically replaced.
- Biopsy: A small tissue sample from the brain is removed during a brain biopsy in order to make a diagnosis. When there is a possibility of a brain tumour or another abnormal growth, this is frequently done. The nature of the tissue is then ascertained from the sample in order to inform future treatment choices.
- Craniectomy: A craniectomy, like a craniotomy, entails the temporary or long-term removal of a portion of the skull. The bone flap may not be replaced right away, unlike a craniotomy, which may allow the brain to swell without being compressed. In cases of severe traumatic brain injuries, strokes, or brain swelling, craniectomies are frequently carried out.
- Deep Brain Stimulation (DBS): DBS is a surgical procedure that is used to treat a variety of neurological conditions, including Parkinson's disease, essential tremor, and dystonia. It entails inserting electrodes into particular brain regions that are connected to a stimulator implanted in the chest. In order to modulate abnormal neural activity and treat symptoms, the device delivers controlled electrical impulses to the brain.
- Vagus Nerve Stimulation (VNS): Although VNS doesn't involve performing a direct brain operation, it does involve implanting a device that stimulates the vagus nerve, a significant nerve connected to the brainstem. When other treatments have failed to control epilepsy or depression, VNS is used.
- Stereotactic radiosurgery: This minimally invasive method uses laser-like radiation beams to precisely target and remove tumours, lesions, and other abnormalities from the body. Small tumours or lesions that are challenging to reach through conventional surgery benefit the most from it.
- Hemispherectomy: A hemispherectomy is when one of the hemispheres of the brain is removed or severed. This extreme procedure, which aims to stop abnormal brain activity from spreading to the rest of the brain, is typically saved for cases of severe epilepsy that do not respond to other treatments.
- Endoscopic procedures: To access and treat brain lesions, tumours, or hydrocephalus (an accumulation of cerebrospinal fluid), minimally invasive endoscopic techniques entail inserting a small incision or natural opening through which a thin, flexible tube with a camera (endoscope) is inserted. Less scarring and quicker recovery times are frequent outcomes of these procedures.
- Shunt Placement: Shunt placement, while not strictly brain surgery, entails inserting a tube to drain surplus cerebrospinal fluid from the brain to another area of the body, frequently the abdominal cavity. This method is frequently employed to treat hydrocephalus.
Risks Associated with Brain Surgery
Here are some of the risks associated with brain surgery:
- Infection: Infections are a significant concern following brain surgery. The surgical site can become contaminated with bacteria, leading to infections in the brain or surrounding tissues. Infections can be serious and may require additional treatment, such as antibiotics or further surgical intervention.
- Bleeding: Blood vessels and delicate brain tissue must be handled during brain surgery. A hematoma, or localised collection of blood, can form during or after surgery as a result of bleeding, which could put pressure on the brain and possibly result in neurological deficits.
- Swelling of the Brain: Brain Edema also known as cerebral Edema, can develop after surgery. Increased pressure inside the skull brought on by swelling may compress brain tissue and affect blood flow, possibly resulting in neurological problems.
- Seizures: Brain surgery increases the risk of seizures by interfering with the brain's normal electrical activity. The severity of seizures can vary, and they may need additional antiepileptic drug therapy.
- Neurological Deficits: There is a chance that the surgery will result in neurological deficits, depending on where it is performed and how much. Changes in motor coordination, speech, memory, and cognitive abilities are examples of these deficits.
- Cerebrospinal Fluid Leakage: The Brain and spinal cord are surrounded and cushioned by cerebrospinal fluid (CSF), which can leak. Accidental CSF leaks following brain surgery can result in headaches, infections, or fluid build-up, among other potential side effects.
- Stroke: A stroke may result from the manipulation of blood vessels during brain surgery. A blood clot or blood vessel rupture can cause a stroke, which may result in neurological damage.
- Anaesthesia Risks: General anaesthesia is required for brain surgery, and there are certain risks anaesthesia carries, such as allergic reactions, breathing problems, and blood pressure changes.
- Functional Impairments: Depending on the intended outcome of surgery, especially when treating epilepsy or removing tumors, functional limitations may result. To balance maintaining brain function with achieving the surgical goal is a challenging task.
- Impact on Patients' Mental and Emotional Health: Patients who have had brain surgery may experience serious psychological and emotional effects. Recovery, rehab, and adjusting to potential changes in cognitive or physical abilities can be difficult processes.
- Postoperative Complications: Following brain surgery, there is a possibility of several complications, including blood clots, pneumonia, or wound infections, which can influence the course of the recovery process.
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now









