Brown Sequard Syndrome
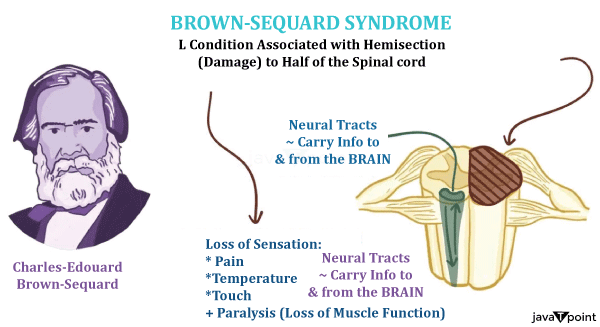
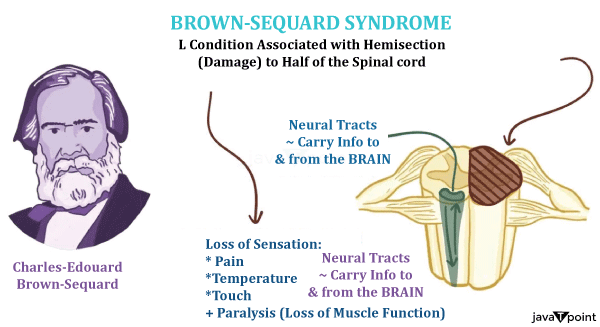
The neurological disorder known as Brown-Sequard Syndrome, which was first described in 1850 by French neurologist Charles-�douard Brown-Sequard, is uncommon but fascinating. It is caused by spinal cord damage. This syndrome illustrates the spinal cord's complex structure and range of functions as a distinct clinical manifestation of spinal cord injury. The Brown-Sequard Syndrome, which is characterized by a distinct pattern of neurological deficits, provides important insights into the complex operations of our nervous system and the difficulties that those who suffer such injuries must overcome.
Typically, tumours or herniated discs that compress or harm the spinal cord cause Brown-Sequard Syndrome. Trauma, such as a stabbing or gunshot wound, can also cause it. The asymmetric spinal cord damage that affects one side of the spinal cord more severely than the other is the cause of the syndrome's distinctive clinical characteristics. There are distinct sensory and motor deficits because of this unequal injury.
Anatomy
Understanding the basic spinal cord anatomy is crucial to comprehending Brown-Sequard Syndrome. The spinal cord, which runs from the brain's base to the lumbar region of the spine, is an essential part of the central nervous system. The vertebral column, which protects it, is made up of 33 vertebrae that are spaced apart by intervertebral discs.
White matter and grey matter make up the spinal cord. While axons in the white matter carry signals from the brain to the rest of the body, the grey matter contains the cell bodies of neurons and is involved in processing sensory data. These axons are organized into tracts, each of which performs a particular task, such as sensory perception or motor control.
The spinal cord is a long, cylindrical bundle of nerves that runs from the brain's base to the lower back. It is essential for the communication of signals between the brain and the rest of the body. The grey matter of the spinal cord is made up of nerve cell bodies, and the white matter is made up of signal-transmitting axons.
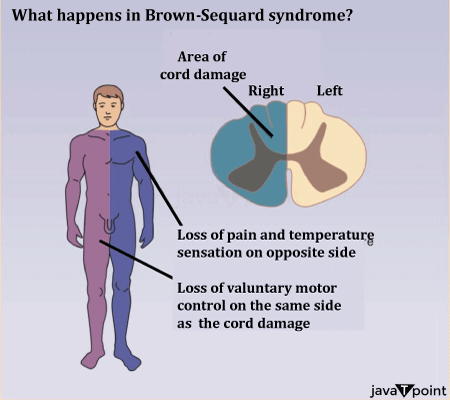
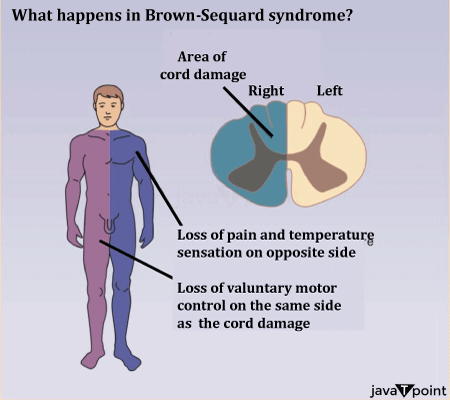
Symptoms of the Disease
Damage to the spinal cord on one side causes the Brown-Sequard Syndrome, which results in neurological deficits. Based on the severity and scope of the injury, different clinical presentations exist. Symptoms are as follows:
- Ipsilateral (Same-Side) Motor Weakness: One of the defining signs of Brown-S�quard Syndrome is skeletal muscle weakness or paralysis on the side of the body where the brain's spinal cord is injured. The reason for this is that one side of the spinal cord is affected, which affects the motor tracts (like the corticospinal tract) in charge of regulating voluntary muscle movements.
- Loss of Proprioception to the Ipsilateral Side: Proprioception is the awareness of one's own body's position and motion. Along with the motor weakness on the same side, Brown-Sequard syndrome also causes proprioception loss. Accordingly, those who are affected have trouble detecting the position and motion of their injured limbs.
- Ipsilateral Vibrational Sense Loss: The spinal cords sensory pathways are what allow the body to detect vibrations. The same side that has motor weakness and a proprioceptive deficit also has a loss of vibratory sensation in Brown-Sequard syndrome. The sensory impairment is exacerbated by this.
- Loss of Pain and Temperature Sensation on the Contralateral (Opposite-Side): One of the most puzzling features of Brown-Sequard Syndrome is the disappearance of pain and temperature sensitivity on the side opposite the motor and sensory deficits. Pain and temperature pathways quickly cross to the opposing side of the spinal cord after entering, which causes this phenomenon.
- Ipsilateral Hyperesthesia: Hyperesthesia is the term for heightened sensitivity to touch or other sensory stimuli. On the same side as the motor weakness and sensory deficits, people with Brown-Sequard syndrome may occasionally experience hyperesthesia. This increased sensitivity, which can be uncomfortable, is thought to be the result of altered sensory processing brought on by the injury.
- Bladder and Bowel Dysfunction: Spinal cord injuries frequently cause the bladder and bowels to stop working normally. People who have Brown-Sequard syndrome may have changes in bowel habits, urinary incontinence, or trouble emptying their bladder. These symptoms need to be managed because they can significantly lower a person's quality of life.
- Sexual Dysfunction: Brown-Sequard Syndrome patients may experience sexual dysfunction because the autonomic nervous system pathways that regulate sexual response are disturbed. Erectile dysfunction in men and trouble initiating orgasm in both sexes can be symptoms of this.
- Spasticity: People with Brown-Sequard syndrome may eventually experience muscle spasticity on the afflicted side. Uncontrollable muscle contractions, stiffness, and spasms are symptoms of spasticity. It may make it more difficult to move around and perform daily tasks.
- Paresthesia: People with Brown-Sequard syndrome may also experience strange sensations on the affected side in addition to the loss of sensory modalities. Paresthesia's like tingling, pins-and-needles, or burning may be experienced.
Diagnosis of the Disease
A spinal cord injury-related pattern of neurological deficits known as Brown-Sequard Syndrome characterizes this uncommon neurological condition. For the syndrome to be properly treated and managed, an accurate and prompt diagnosis is necessary.
- Medical History: A thorough medical history is frequently the first step in the diagnostic process. Patients are questioned regarding when their symptoms first appeared, any recent traumatic experiences or injuries, existing medical conditions, and prior operations or treatments. Having this data on hand enables medical professionals to place the patient's current neurological presentation in context.
- Neurological Examination: Brown-S�quard Syndrome must be diagnosed with the help of a thorough neurological examination. The test evaluates several facets of motor and sensory function, such as muscle power, coordination, reflexes, and sensory perception.
- Motor Examination: Throughout the body, the examiner measures the muscle tone and strength in various muscle groups. Brown-S�quard Syndrome is suspected when there is weakness or paralysis on one side of the body, especially when it occurs in a pattern that fits the syndrome.
- Sensory Examination: The sensory examination involves evaluating several senses, such as proprioception (a sense of where the body is in space), temperature, pain, and light touch. The loss of proprioception, vibratory sense, and light touch along with the loss of pain and temperature sensation on the contralateral side (the opposite side) are the distinguishing characteristics of Brown-S�quard syndrome.
- Magnetic Resonance: Imaging tests are essential for diagnosing Brown-S�quard Syndrome and figuring out what caused the spinal cord injury, including magnetic resonance imaging (MRI). The best imaging technique is MRI because it gives clear, detailed pictures of the spinal cord and its surroundings. The location, size, and type of the spinal cord lesion, such as a herniated disc, tumour, or traumatic injury, can be determined by an MRI.
- Computed Tomography (CT) Scan: A CT scan may be used in some circumstances, particularly in the emergency room, to evaluate spinal cord injuries. CT scans are useful for locating spine-related fractures or skeletal anomalies that may be contributing to the injury.
- Myelography: During myelography, a contrast dye is injected into the spinal canal, after which a series of X-ray images are taken. Particularly in cases where MRI is contraindicated or not available, this procedure can aid in the visualisation of abnormalities in the spinal cord or surrounding structures.
Tests for Electrophysiology
In some circumstances, electrophysiological tests may be used to examine nerve conduction and gauge the spinal cord's performance. These tests can offer additional data to support the Brown-Sequard Syndrome diagnosis:
- Somatosensory Evoked Potentials (SSEPs): Somatosensory Evoked Potentials (SSEPs) involve stimulating sensory nerves and observing the electrical brain responses. This test may be used to determine the health of sensory pathways and to confirm the loss of sensory modalities linked to Brown-Sequard syndrome.
- Electromyography (EMG) is a technique for analyzing the electrical activity of muscles. It can be helpful in determining the degree of denervation or abnormal muscle behaviour, as well as the extent of motor nerve involvement.
Alternative Diagnosis
Like Brown-Sequard Syndrome, several other neurological disorders and spinal cord disorders can manifest symptoms. To exclude these conditions and make a precise diagnosis, a differential diagnosis is essential:
- Transverse myelitis: It is an inflammatory condition that affects the spinal cord and can result in weakness, sensory loss, and other neurological deficits. As their treatment and underlying causes differ, it is crucial to distinguish it from Brown-Sequard Syndrome.
- Syringomyelia: Syringomyelia is a condition that causes fluid-filled cavities to grow inside the spinal cord. It can result in motor deficits and sensory disturbances, frequently bilaterally.
- Hemiparesis: Hemiparesis is the term used to describe weakness or paralysis on one side of the body. It is typically unrelated to the sensory deficits present in Brown-Sequard Syndrome. It frequently results from a stroke or another condition that affects the brain.
Treatment
Quick Care
The initial treatment for Brown-Sequard syndrome concentrates on stabilizing the patient's condition, attending to any life-threatening wounds, and stopping further spinal cord damage. Acute care practices consist of:
- Immobilization: In order to stop further damage, the spine must be stabilised. To immobilise patients while the severity of the injury is assessed, cervical collars or spinal boards are frequently used.
- Support for the Airway and Breathing: Respiratory function may be impaired in cervical spinal cord injury cases. To keep patients breathing and oxygenating properly, patients may need to be intubated and given mechanical ventilation.
- Cardiovascular Support: Blood pressure control is essential to avoiding complications from autonomic dysfunction, which can happen in spinal cord injuries. To keep blood pressure stable, medication and fluid management may be necessary.
Rehabilitation
The focus switches to rehabilitation after the patient's condition has stabilised because it is crucial to the recovery of those with Brown-S�quard Syndrome. The following elements are frequently included in rehabilitation because it aims to maximise function and independence:
- Physical therapy: Patients receive physical therapy to increase their muscle strength, coordination, and mobility. The patient's specific deficits and goals are taken into account when designing rehabilitation exercises and activities.
- Occupational Therapy: Patients who have lost the ability to dress, groom, or cook for themselves can benefit from occupational therapy. They might also offer adaptive tools and methods.
- Assistive Devices: Depending on the severity of the neurological deficits, patients may need assistive devices to help them move around, such as braces, canes, walkers, or wheelchairs.
- Management of the Bowels and Bladder: Bowel and bladder dysfunction are common in people with Brown-S�quard syndrome. Specialists in rehabilitation can teach methods for handling these problems, such as catheterization and bowel programmes.
- Pain management: Pain in Brown-S�quard syndrome can be a major concern. Medication, physical modalities (such as heat or cold therapy), and relaxation techniques are some examples of pain management techniques.
- Psychological Support: Dealing with the psychological and physical effects of spinal cord injury can be difficult. Counsellors or psychologists can offer emotional support as well as coping mechanisms.
Surgery Activities
In some cases of Brown-S�quard syndrome, surgery may be required to stabilise the spine or treat the spinal cord injury's underlying cause. The following surgical options are available:
- Decompressive surgery: It may be performed to remove the source of compression and decompress the spinal cord if the spinal cord injury was brought on by a herniated disc, tumour, or another compressive lesion.
- Spinal Fusion: In cases of spine instability or fractures, spinal fusion surgery may be required to stabilise the affected vertebral segments.
- Tumour Resection: If a spinal tumour is the cause of the syndrome, surgical removal of the tumour may be necessary. Radiation or chemotherapy may then be used as additional treatments.
- Intrathecal Baclofen Pump: Patients with severe spasticity occasionally benefit from having an intrathecal baclofen pump implanted. Through the direct delivery of a muscle relaxant to the spinal cord, this device can lessen spasticity and increase mobility.
Continued Management
Because Brown-Sequard Syndrome is a chronic condition, ongoing care is necessary to meet the patient's changing needs. Important elements of long-term management include:
- Ongoing Rehabilitation: Rehabilitation should be a continuous process with regular assessments to gauge progress and alter treatment plans as necessary.
- Regular Medical Follow-Up: Patients with Brown-S�quard Syndrome should schedule routine follow-up visits with their medical professionals to monitor their general health and address any new or developing problems.
- Pain management: People with Brown-S�quard syndrome may find it difficult to manage chronic pain. Physical therapy, medication, and interventional pain procedures are all possible long-term pain management techniques.
- Care for the Bowel and Bladder: To avoid complications like skin deterioration and urinary tract infections, it is essential to effectively manage bowel and bladder dysfunction. Patients must adhere to suggested bowel and bladder programmes and practise good hygiene.
- Adaptive Strategies: Patients may need new adaptive strategies and assistive devices as they adjust to their condition to improve their independence and quality of life. The ability to cope with a spinal cord injury can have a significant impact on one's mental health.
- Emotional and Psychological Support: It's crucial to have access to ongoing psychological support and counselling when dealing with emotional difficulties.
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now









