Cardiac Output DefinitionCardiac Output (CO) is mainly known as the amount of blood pumped by the heart through the circulatory system within our body in one minute. It is the product of the heart rate (the number of heartbeats per minute) and the stroke volume (the amount of blood pumped by the heart with each beat). 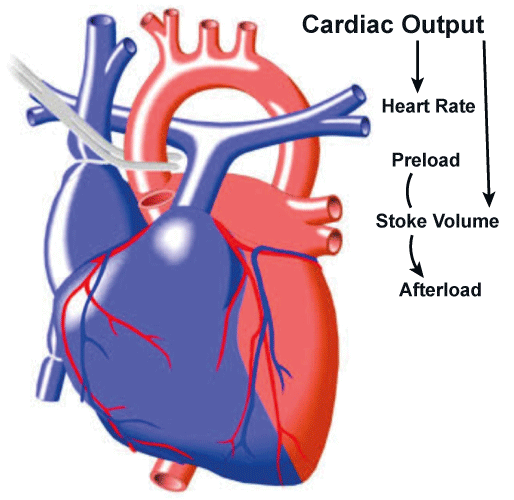
Cardiac output typically helps to measure how much blood the heart pumps in one minute, typically expressed in litres per minute (L/min). It is an important physiological indicator of the heart's ability to supply the body with the nutrients and oxygen it needs. It is also an important physiological indicator to measure the health of the heart because it shows how well the heart can deliver nutrients and oxygen to the body. It is affected by several things, including physical exercise, stress, and illness conditions, including heart failure. It is frequently used in clinical settings to gauge how well the heart is working, and it may be assessed using various techniques, including echocardiography and thermodilution procedures. The heart is the muscular organ that functions as the body's crucial part and pumps blood throughout the body. The heart must be able to modify its output in response to shifting demands to maintain a proper blood flow to the tissues. For example, the body's need for oxygen increases during certain physical activities, forcing the heart to pump more blood to meet the demand. On the other hand, when the body is at rest, its need for oxygen decreases, and cardiac output adjusts that requirement accordingly. Determinants of Cardiac OutputCardiac output is generally determined by two main factors, namely heart rate and stroke volume. Heart rate usually refers to the number of times the heart beats per minute, and stroke volume is the amount of blood pumped out of the heart with each beat. Heart RateThe heart rate is regulated by the autonomic nervous system, which consists of two branches: the sympathetic and parasympathetic nervous systems. The sympathetic nervous system controls the heart to beat faster and harder, while the parasympathetic nervous system has a different effect; it typically slows down the heart rate. The balance between these two systems constantly shifts in response to various factors such as stress, exercise, and disease. Stroke VolumeStroke volume is classified by several factors, including the size and strength of the heart, the volume of blood returning to the heart (preload), and the resistance to blood flow in the arteries (afterload).
Cardiac Output RegulationThe body maintains cardiac output by regulating heart rate and stroke volume. For example, during exercise, the sympathetic nervous system is activated, increasing heart rate and stroke volume, which increases cardiac output to meet the increased oxygen demand of the muscles. Conversely, during rest periods, the parasympathetic nervous system is activated, decreasing heart rate and stroke volume, which decreases cardiac output. Clinical SignificanceCardiac output is an important clinical parameter often used as an indicator of the effectiveness of cardiac function. A decrease in cardiac output can result in symptoms such as fatigue, shortness of breath, and decreased exercise tolerance. Cardiac output can be measured using various methods, including echocardiography, thermodilution techniques, and Doppler ultrasound. Changes in cardiac output can be seen in various disease states, including heart failure, myocardial infarction, and sepsis. How was cardiac output invented?Cardiac output as a concept was not "invented" but established or rather analyzed over time through the work of various researchers and physicians. The concept of cardiac output can be traced back to the late 19th century when French physiologist Etienne-Jules Marey developed a method for measuring blood flow velocity using a sphygmograph. In the early 20th century, British physiologist Ernest Starling proposed the "law of the heart", which stated that the heart would pump out as much blood as was returned from the veins. This concept was later expanded upon by American physiologist Otto Frank, who developed the "Frank-Starling law", which described the relationship between preload (the amount of blood returning to the heart) and stroke volume (the amount of blood ejected from the heart with each beat). The development of modern techniques for measuring cardiac output began in the mid-20th century. In 1953, Swedish physiologist Sven Ingvar Seldinger introduced the technique of catheterization, in which a thin flexible tube is inserted into a blood vessel and guided toward the heart. This technique allowed the measurement of various hemodynamic parameters including cardiac output. In the 1970s, thermodilution techniques were developed for measuring cardiac output. This technique involves injecting a known volume of cold saline solution into a vein and then measuring the temperature of the blood as it flows past a thermistor located in the pulmonary artery. By analyzing the temperature changes, cardiac output can be calculated. Overall, the development of the concept of cardiac output and the techniques for measuring it has resulted from a long and ongoing process of scientific inquiry and innovation, driven by the need to understand the functioning of the cardiovascular system better and to diagnose and treat various diseases and conditions. Calculating Cardiac OutputCardiac output (CO) is the volume of blood that the heart pumps per unit of time, usually measured in litres per minute. The main role of the heart is to pump blood to all the body parts to supply nutrients and oxygen and also help remove waste products. Cardiac output plays a crucial role in maintaining adequate tissue perfusion, essential for the normal functioning of various organs in the body. The formula for cardiac output is defined below: CO = heart rate (HR) x stroke volume (SV) Here, heart rate is the number of times the heart beats per minute, and stroke volume is the amount of blood ejected by the heart in each beat. For instance, suppose that a person has a heart rate of 70 beats per minute and a stroke volume of 70 millilitres per beat. In that case, the cardiac output can be calculated as below: CO = 70 beats/minute x 70 mL/beat CO = 4.9 L/minute Importance of Cardiac OutputCardiac output, a key physiological indicator, measures how much blood the heart pumps in a given time. It is an important measurement because it shows how well the heart can provide oxygen and nutrients to tissues such as the brain, muscles, and organs. Some of the important reasons why cardiac output is essential are discussed below:
Overall, cardiac output is a crucial parameter that reflects the ability of the heart to deliver oxygen and nutrients to the body's tissues. It is important in the diagnosis and treatment of heart disease, as well as in monitoring patients during surgery and assessing one's exercise capacity. By understanding the concept of cardiac output, clinicians can better diagnose and treat various health problems and help patients achieve optimal health and well-being. In highly trained athletes, cardiac output can increase to 40-50 litres per minute. ComplicationsThe complications associated with the cardiac output can be explained in several contexts, including:
In summary, cardiac output is crucial in maintaining tissue perfusion and oxygenation in various physiological and pathological contexts. Monitoring and managing cardiac output is essential in diagnosing and managing various cardiovascular and systemic diseases. The Function of Cardiac Output in CardiologyIn cardiology, cardiac output (CO) is a crucial measurement used to assess the heart's ability to pump blood and to evaluate various cardiovascular disorders. The primary function of cardiac output in cardiology is to estimate the blood flow through the cardiovascular system. Following are some of the notable functions of cardiac output in cardiology: Diagnosis and Assessment of Cardiovascular DisordersCardiac output is a critical measurement to diagnose and evaluate cardiovascular disorders, including heart failure, valve disorders, and cardiogenic shock. By measuring cardiac output, doctors or physicians can assess the heart's ability to pump blood, identify abnormalities, and monitor the effectiveness of treatments. Guide Therapeutic InterventionsCardiac output is often used to guide therapeutic interventions in patients with cardiovascular disorders. For example, medications such as inotropes and vasodilators can increase cardiac output, while diuretics and beta-blockers can decrease it. By monitoring cardiac output, physicians can adjust therapies to optimize cardiovascular function and improve patient well-being. Assessing Hemodynamic StabilityCardiac output is a crucial measurement to assess a patient's hemodynamic stability, particularly in critically ill patients. Low cardiac output can lead to inadequate tissue perfusion and organ dysfunction and failure. By monitoring cardiac output, clinicians can identify and manage hemodynamic instability promptly. Monitoring Response to InterventionsCardiac output monitors the response to various interventions, including medications, fluid resuscitation, and mechanical circulatory support. By monitoring changes in cardiac output, clinicians can evaluate the effectiveness of interventions and adjust them as needed.
Next TopicCarnivore Definition
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










