Hypoxemia DefinitionLack of oxygen results in instant death as oxygen is a crucial component for human existence. Respiratory failure is a condition when the respiratory process is unable to perform either one or both of its gas exchange actions, which include oxygenation and the exhalation of gases such as carbon dioxide from mixed blood that is venous. Hypoxemia, or a severe reduction in blood oxygenation, is one of the primary markers of such failure. Comparable to other physiologic systems, the complete oxygenation process is dynamic. The human lung can only react to harm in a small number of different ways, much like other organ systems. As an outcome, five essential pulmonary mechanisms-ventilation-perfusion mismatch, alveolar hypoventilation, diffusion impairment, right to left shunt, also or diffusion-perfusion irregularity-lead to arterial hypoxemia. Defining Hypoxemia.A decrease in bloodstream oxygen levels is referred to as hypoxemia. A shortage of oxygen can be detected in the blood, which implies the amount of oxygen is below the usual range. In simple terms, it occurs when your blood's oxygen levels are below normal. You risk having an unbalanced body if your blood oxygen levels are too low. A person who has low blood oxygen levels is said to be hypoxemic. The lungs constitute how oxygen enters circulation. Little air sacs called alveoli in your lungs, where you breathe in, get oxygen from the surrounding air. The oxygen gets into the body via blood arteries (capillaries) that move near to the alveoli. In the end but not least, oxygen gets to your tissues via your blood. 
The inability to breathe in enough oxygen or the inability of the oxygen you breathe in to reach your blood may both result in hypoxemia. For your blood to contain adequate oxygen, air & blood circulation are equally necessary. This is why having lung or heart illness makes you more likely to get hypoxemia. Hypoxemia can trigger minor symptoms or fatal outcomes, depending on its intensity and duration. Headaches and breathing problems are two symptoms that are mild. Hypoxemia may, in extreme situations, affect how the brain and the functioning of heart. It could result in hypoxia or an inadequate supply of oxygen to your body's tissues and organs. Respiratory failure which is "acute" in nature can result from hypoxemia that lasts just for a short period of time. You might have heard the phrase "chronic respiratory failure" used when it's a long-term issue that lasts for months or years. How Much Arterial Oxygen Is Considered Normal?A number of medical disorders may be diagnosed by measuring the quantity of oxygen in your blood. This may be accomplished in a number of ways. A portion of the blood is collected from an artery, generally from the wrist, to perform an arterial blood gas (ABG) test, which may determine the levels of oxygen and carbon dioxide within the blood. Blood travels via arteries, which are blood vessels, to reach the tissues and organs of the body with oxygen-rich blood. The outcomes of an ABG test can give your doctor information about the amount of oxygen in the blood which is presently being transported to the tissues in your body since the sample of blood is taken from an artery. They may be informed of the efficiency of the carbon dioxide removal from your blood by it as well. Pulse OximeterYour doctor may suggest using a pulse oximeter if you experience difficulty in breathing or are suffering from diagnosed lung or heart disease. An electronic instrument known as a pulse oximeter, sometimes known as a Pulse Ox, observes the saturation level of oxygen carried by your red blood cells. It's possible to attach a pulse oximeter to the tips of your fingers, forehead, nose, foot, ears, or toes. Then, the gadget may either be reused or thrown away. Given that pulse oximetry equipment may be costly and reusable if you use it at home, you should consult your doctor before discarding it. The pulse oximeter may provide false or inconsistent readings if you suffer from poor circulation, uneven skin coloration, thick skin, presently consume tobacco products, your body tone is chilly, you use dark nail enamel, long, synthetic nails, or your fingers are dirty. Because of this, it's not advisable to gauge your level of health only based on the results of a pulse oximeter. A typical reading ranges from 95 and 100 percent for the majority of individuals, however, it might be lower if you have a lung ailment or reside at a high altitude. Consult the doctor if you take an at-home pulse oximeter and obtain an oxygen saturation of 92 percent or below if you are otherwise healthy. Distinguishing Hypoxemia from HypoxiaEven though the words hypoxemia and hypoxia frequently come up collectively, they are not the same thing. When arterial oxygen tension (PaO2), which should be between 80 and 100 mmHg, is below normal, it is said to have hypoxemia. On the contrary hand, hypoxia can be defined as a decrease in tissue-level oxygen supply and is not immediately evaluated by laboratory measurement. Hypoxia is often indicated by the presence of hypoxemia. Hypoxia may not exist in hypoxia patients, nevertheless, if they increase oxygen supply to make up for their low PaO2. Usually, this is done by either slowing tissue oxygen consumption or speeding up cardiac output (by elevating the heart rate). On the other hand, people who do not exhibit hypoxemia symptoms may nevertheless be hypoxic if the tissues are unable to utilize oxygen effectively or if the oxygen supply to the tissues is impeded. The first type of action is best shown by cyanide poisoning, which prevents tissues from undergoing aerobic metabolism. Although hypoxemia is undoubtedly the most frequent cause of tissue hypoxia, it is important to get an accurate diagnosis since it is easily curable. Which Factor Triggers Hypoxemia Most Frequently?The primary cause of hypoxemia is a underlying disease that interferes with breathing or blood flow (such as heart or lung issues). Hypoxemia may have many different causes. Certain drugs have the potential to impede breathing and cause hypoxemia. When oxygen levels in the blood fall while you're sleeping, it's known as nocturnal hypoxemia. Sleep apnea and moderate lung illness may cause this. It may be difficult to breathe while you're in the mountains since being at a high altitude may also induce hypoxemia. 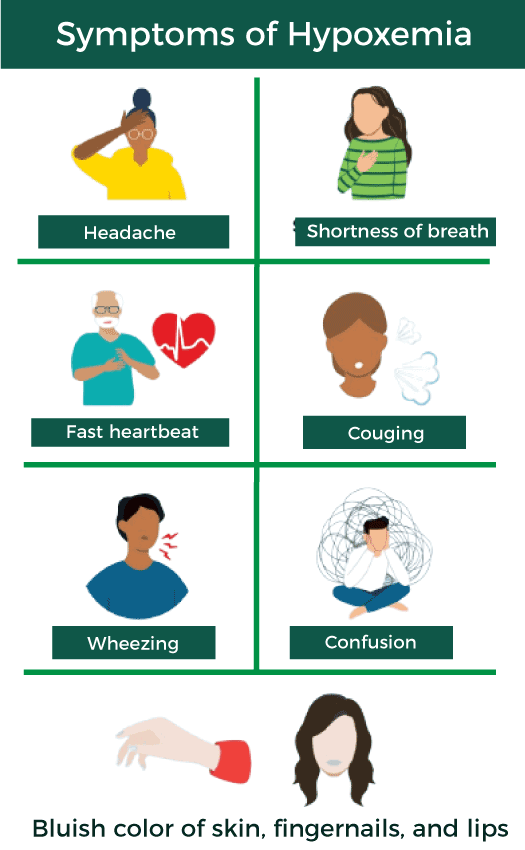
Hypoxemia may be caused by several medical problems, such as: 1. Acute Respiratory Distress Syndrome (ARDS)A hazardous lung damage brought on by sepsis, pneumonia, the coronavirus (COVID-19), and various other issues is known as acute respiratory distress syndrome (ARDS). After the triggering incident, ARDS often manifests within a few hours to a few days and may deteriorate quickly. Patients with ARDS may need to be placed in an intensive care unit (ICU) and put on a ventilator to assist with breathing. 2. AnaemiaWhen the number of healthy red blood cells necessary to transfer oxygen to your body's organs is insufficient, anaemia develops. As a consequence, it's normal to have symptoms such as weakness or exhaustion as well as a cold. Iron-deficiency anaemia is the most prevalent kind of anaemia, however there are numerous others. By include more iron in your diet, you may start to reduce the symptoms of this kind of anaemia. 3. BronchitisThe condition known as bronchitis occurs when the bronchi and trachea, the airways that lead to the lungs, become irritated and mucus-filled. As your body attempts to expel the mucus, a persistent cough develops. Your cough may persist for up to two weeks. Viruses are often the cause of acute bronchitis, which resolves on its own. Although chronic bronchitis may be treated, it never completely goes away. 4. COPD (Chronic Obstructive Pulmonary Disease)An assortment of diseases known as chronic bronchitis and emphysema are included in chronic obstructive pulmonary disease (COPD). COPD gradually makes breathing more difficult. While lung damage cannot be reversed, you can cope with the symptoms by making a few adjustments to your lifestyle and medications. 5. Congenital Heart DiseaseA structural abnormality in the heart that exists from birth is known as congenital heart disease (CHD). It may be discovered at any moment throughout life, including just before delivery and just after. CHD may have many different forms. The kind of defect and how severe it is determining the symptoms and course of therapy. All throughout their lives, a person with CHD has to see a cardiologist often. 6. EmphysemaLung illness known as emphysema. Emphysema generally comes through smoking, however it may also be brought on by other factors such as pollution in the air and chemical fumes. Breathing difficulty, coughing, and exhaustion are symptoms. Imaging and respiratory examinations may help your doctor determine whether you have emphysema. The course of treatment involves both medicine and quitting smoking. What Are The Five Reasons For Hypoxemia?Ventilation-perfusion (V/Q) mismatch, hypoventilation, low ambient oxygen, and right-to-left shunting are the five types of hypoxemia-causing disorders that may be brought on by problems with heart and lung function.
Blood is circulated during perfusion, which is different from ventilation, which is air that a person inhales and exhales. A common ventilation/perfusion (V/Q) proportion is slightly around 1. Both airflow into the lungs (ventilation) and the flow of blood to the lungs (perfusion) are necessary for oxygen to reach your blood. If one of them isn't functioning, you'll either have lots of oxygen in your lungs yet insufficient blood flow to absorb it, or the opposite will be true. When a portion of the lungs receives oxygen but no blood flow or receives blood flow but no oxygen, this is known as a V/Q mismatch. Based to the available data, hypoxemia is often brought on by a V/Q mismatch.
When breathing is not enough to keep up with the body's need for oxygen and carbon dioxide exchange, hypoventilation occurs. Low levels of oxygen and high levels of carbon dioxide (CO2) are present in the blood during hypoventilation. As a consequence, hypoxemia is often prevalent, particularly during sleeping. Breathing patterns that are weak and sluggish may be seen in someone who is hypoventilating.
When blood from the right side of the heart flows into the left side without exchanging oxygen or carbon dioxide, this is referred to as a shunt. Your heart receives deoxygenated blood from the right, pumps it to your lungs where it receives oxygen, then receives it back from the left where it is pumped to your body. Deoxygenated blood may go to your tissues without first receiving oxygen in your lungs in certain individuals when it is pushed to the left side of your heart. Right-to-left shunting is the medical term for this condition, which is often brought on by a cardiac condition.
When the oxygen transmission between the alveoli and the capillaries is disrupted, it leads to diffusion impairment. As oxygen diffuses into capillaries, it enters the blood vessels in the lungs' alveoli, which are sacs wherein gas exchange occurs. The ability of oxygen to transfer from your lungs to your blood vessels may at times be compromised, despite having sufficient blood flow and ventilation. Emphysema, lung scarring, or illnesses that reduce the blood flow between the lungs and the heart may all contribute to diffusion impairment.
Hypoxemia might occur as a consequence of low surrounding PaO2. For instance, at higher elevations, the partial pressure of oxygen is lower. Your blood cannot get the necessary amount of oxygen for your body to function if there is insufficient oxygen in the air you are breathing. In comparison to places at lower elevations, higher-elevation locations possess less oxygen in the air. How Is Hypoxemia Detected Medically?Your doctor will do a physical checkup and monitor to your breathing and heartbeat to determine the presence of hypoxemia. These organs' abnormalities may indicate low blood oxygen levels. Your doctor could also examine you to discover whether you have blue fingernails, skin, or lips. Your healthcare professional will do tests to determine your oxygen levels, which may include:
How Does Hypoxemia Get Treated?Medications or alternative treatments may help increase your blood oxygen level, depending upon the root cause of your hypoxemia. Your doctor might use oxygen storage tanks or concentrators of oxygen to deliver "supplemental oxygen" to assist boost oxygen levels. Depending on how severe the illness is, they may need to be taken continually or just when exerted. Healthcare professionals can use a ventilator-a machine that breathes for you-in the event of severe hypoxemia, particularly when it occurs in conjunction with acute respiratory distress syndrome. Additional drugs or treatments may be used to treat refractory hypoxemia, which is hypoxemia that doesn't go away on its own. The following are examples of treatments that target the underlying cause:
ConclusionDespite the fact that hypoxemia can prove life-threatening, it is curable when medical care is received right away. In other cases, such as overnight if you have sleep apnea, it may also occur sporadically without any evident signs. It's vital to understand your risk and the preventive steps you may take since this can eventually harm your heart.
Next TopicNosocomial Infections Definition
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










