Nursing Process DefinitionIda Jean Orlando started creating the nursing approach in nursing care today in 1958. Orlando's idea states that the patient's behavior initiates the nursing process. The nurse can determine the patient's requirements by analyzing and diagnosing the behavior. 
The five elements of the nursing process serve as a systematic schedule for client-centered care by including the essential concepts of critical thinking, client-centered treatment methods, goal-oriented activities, evidence-based practice (EBP) recommendations, and nursing intuition and ADPIE stands for assessment, diagnosis, planning, implementation, and evaluation. What happens during nursing procedures?
A systematic, logical planning strategy that leads all nursing actions toward delivering comprehensive, patient-focused care is the definition of the nursing process. The procedure of nursing, which is a form of scientific reasoning, requires the nurse to employ critical thinking to provide the patient with the best care possible. What benefits does the nursing process offer?The following objectives are part of the nursing process:
Aspects of the nursing process
The following aspects make the nursing process unique: 1) Patient-centredAccording to the distinctive nursing method, a patient's requirements, preferences, and values must be respected and considered when providing care. The nurse serves as the patient's advocate by defending the patient's right to make informed decisions and upholding patient-centred participation in healthcare. 2) InterpersonalThe nursing process acts as the foundation for the therapeutic process, allowing the nurse and patient to respect one another as different persons and benefit from their interactions. It entails the nurse and patient interacting with one another to achieve a common objective. 3) CollaborativeThe nursing process encourages open communication, respect for one another, and collaborative decision-making to offer top-notch patient care in nursing and inter-professional teams. 4) Both cyclical and dynamicEach step of the nursing process interacts with and is impacted by the others in a dynamic, cyclical manner. 5) Critical thinking is necessaryNurses must use critical thinking, a crucial talent, to identify client problems and carry out remedies that will result in good care results. Nursing Procedures in Steps
The nursing procedure includes assessment, diagnosis, planning, execution, and evaluation. The acronym ADPIE makes it easy to recall the steps in the nursing procedure. Nurses must follow the procedure step-by-step. However, individuals learn how to bounce between the many stages of the nursing process as their critical thinking skills develop via experience. The nursing process comprises overlapping, ongoing subprocesses rather than distinct procedures. The nurse not only understands nursing diagnostics and their definitions but also spreads the knowledge of the distinguishing characteristics and behaviours of the diagnoses, the contributing factors to the chosen nursing diagnosis, and the therapies appropriate for treating the diagnoses. 1. Assessment: What data is available, according to the Assessment?
Assessment is the first stage of the nursing process. The patient's health condition is gathered, put in order, verified, and documented. This information may be gathered in several ways. A nurse's first Assessment of a patient's health concerns and physiological, psychological, and emotional states is required. The patient's response to health conditions or sickness and their competence to manage their demand for medical treatment are also anticipated to be entered into a database. Changes to the curriculum focused on concepts are necessary since the Assessment depends on critical thinking abilities. A. Gathering information The practice of acquiring information on the patient's condition is known as data collection. The process must be time-consuming and continual while obtaining data to ensure you get all the important consumer information. B. Variety of Data Data can be verbal and nonverbal, but it often falls into one of two categories: objective or subjective. C. Objective Data or Signs The following are some examples of objective data: vital signs, intake and output, height and weight, body temperature, pulse, respiration rates, blood pressure, weeping, lung sounds, an enlarged belly, edema, skin color, and the presence of diaphoresis. They are clear, quantitative, concrete truths gained by the senses, such as sight, touch, smell, or hearing, compared to a predetermined standard. D. Details about the person or symptoms A patient's shared emotions, perceptions, thoughts, sensations, or worries, including their attitudes, beliefs, and values, as well as how they perceive their health problem and life events, are all regarded as subjective data. E. Verbal Data Verbal data includes spoken or written information, such as declarations made by the customer or a secondary source. To identify challenges with verbal data, such as slurring, voice tone, aggressiveness, anxiousness, trouble finding the appropriate term, and flight of ideas, nurses must have good listening skills. F. Nonverbal data The patient's body language, overall look, facial expressions, gestures, eye contact, and attire are examples of nonverbal data or observable acts that convey a message without words. Due to the possibility that someone's body language may not reflect what they truly think or feel, nonverbal information can occasionally be more helpful than verbal information. Nonverbal data collection and analysis can support verbal data collection efforts and provide an understanding of the patient's real emotions. G. Data Sources Data might come from primary, secondary, or tertiary sources. The patient is the primary source of information, whereas secondary sources include the patient's relatives, parents, other healthcare providers, records and reports, laboratories, and diagnostics. H. Main Source A client is a sole person who can supply subjective data and is the only major data source. The main information is everything a patient tells or discloses to the medical staff. I. Secondary Source Secondary data is information from a source other than the patient but is included in the patient's information. In cases where a patient is unable to speak for themselves and is lacking in knowledge and awareness, information from family members or close friends is considered as a secondary data source. Secondary data sources include the patient's records and assessment information from additional nurses or healthcare professionals. J. Tertiary Source Tertiary sources of information are those that come from sources that are not relevant to the customer. Some examples of tertiary data are information from textbooks, medical and nursing publications, drug handbooks, surveys, and policy and procedure manuals. Data Collection Methods
The three basic techniques for gathering data are physical examinations, health interviews, and observation. A. Medical Interview Interviews are the most typical method for acquiring crucial information. A discussion or intentional communication to obtain or provide information, identify issues of shared concern, evaluate change, impart knowledge, offer assistance, or offer counselling or therapy is known as an interview. The nursing health history, a component of the nurse entrance assessment, is one instance of an interview. Rapport must be created throughout this stage of the nursing process since patient involvement is usually the most intense. B. Visual Inspection In addition to conducting interviews, nurses will do physical examinations, consult a patient's medical history, ask about their family history, and make general observations to collect assessment data. An accurate diagnosis, better planning, better actions, and better evaluation would be made possible later on by establishing an effective physical examination. C. Observation The five senses (seeing, touch, hearing, smell, and taste) are used as part of the observation, a method of evaluation, to gather data about a client. The client's surroundings, major connections, functionality, and looks are all addressed in this data. Most of the senses are used during careful observation, including the sense of smell, hearing or auscultating lung and heart sounds, feeling the pulse rate, and feeling other perceptible skin deformations, even though nurses primarily examine through sight. D. Data Validation Validation is the process of confirming the data's accuracy and verification. By "double-checking," a method for validating observations, the nurse can carry out the following tasks: 1) Assures the accuracy, completeness, and double-checking of assessment data. For instance, a client with no history of hypertension has a measurement of 210/96 mm Hg during a normal check by the nurse. The nurse should retest the blood pressure and, if required, utilize other equipment to confirm the reading or have someone else conduct the exam to authenticate the findings. 2) Verify the validity and accuracy of all relevant accurate and subjective data. For instance, it is necessary to compare the client's sense of "feeling hot" with the reading of their body temperature. 3) Make sure the nurse doesn't conclude without sufficient evidence to back it up. Until she reads about the physical changes that come with age, a nurse believes that the small, purple, or bluish-black swellings under the tongue of an older adult client are abnormal. 4) Obtain additional information that may have yet to be noticed. For instance, the nurse is enquiring about the client's 34-year-old sensitivity to prescription or over-the-counter medicine. And what would occur if he took this medicine? 5) Recognize the difference between clues and inferences. The patient's remarks and what the nurse can see, hear, feel, smell, or measure are all examples of cues that the nurse can immediately observe as subjective or objective information. However, the nurse's interpretation or conclusions, referred to as inferences, are based on the evidence. For instance, the nurse could determine that the incision is infected based on its symptoms that it is red, hot, and swollen. Data Documentation
Once all relevant data has been acquired, data may be recorded and organized. Excellent record-keeping is essential to ensure all the information obtained is documented, explained, and available to the healthcare team for use in Assessment. 2. Diagnosis
Diagnostic nursing is the second phase in the nursing process. The nurse will evaluate all the information to ascertain the patient's condition and needs. Data analysis, the identification of health problems, risks,and strengths, as well as the formulation of diagnostic assertions on the possibility of a patient's or existing health problem,are all part of the diagnostic process. A patient may occasionally obtain many diagnoses. Planning and executing patient care are made simpler when a nurse's diagnosis is made using clinical judgment. 3. Planning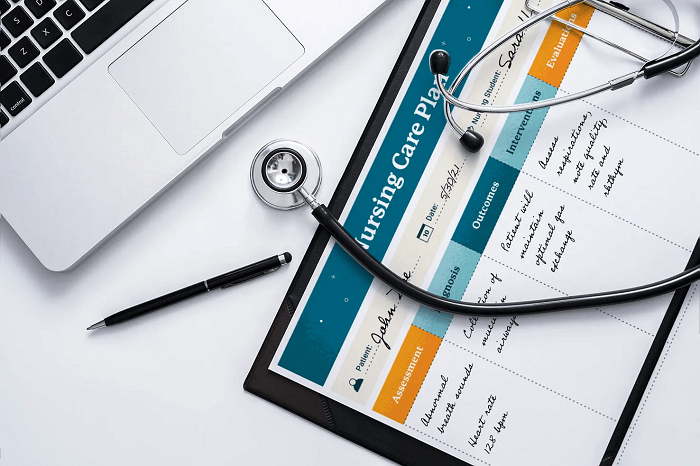
Planning is the third step of the nursing process. It provides direction for nurse intervention. Once the patient, overseeing doctors, and the nurse have agreed on the diagnosis; the nurse will plan a course of treatment that considers both short- and long-term goals. Each issue is dedicated to a specific, quantifiable objective with an anticipated beneficial outcome. According to the principles of evidence-based practice (EBP), goals and outcomes that directly affect patient care are developed during the planning phase. These patient-specific goals and their accomplishment help to guarantee an excellent result. Nursing care plans are essential throughout this stage of achievement of objectives. Care plans provide guidelines for providing personalized care according to a person's specific needs. Creating a treatment plan is influenced by the overall illness and any other medical conditions. Treatment plans improve the coordination of treatment, documentation, payment, and continuity of care throughout the healthcare system. 1) Different Forms of Planning The initial patient's reactions triggerthe start of planning, which lasts until the nurse's and the patient's link is broken, preferably when the patient is released from the healthcare facility. 2) Initial Planning The nurse who does the admission evaluation begins the planning process. The same nurse often created the initial detailed plan of treatment. 3) Continuous Planning Every nurse who assists the patient engages in continual planning. A nurse can further individualize the initial treatment plan by acquiring more data regarding the patient's responses to treatment. At the beginning of a shift, an ongoing care plan is also initiated. Planning continuously enables the nurse to:
4) Planning for Discharge Discharge planning is the process of anticipating and preparing for obligations following release. Nurses must complete the following tasks to guarantee continuity of care:
5) Planning a Nursing Care Program An approved nursing care plan (NCP) method properly determines present needs and acknowledges upcoming requirements or concerns. Care plans improve communication between nurses, their patients, and other medical providers to accomplish healthcare goals. To keep the standard and consistency of patient care high, nurse care planning is a need. 4. Implementation
The nurse executes the treatment plan throughout the nursing process implementation phase. It entails acting, carrying out acts, and concluding the nursing interventions defined in the care plan. The medical staff will typically begin by providing any required medical care. Interventions should focus on achieving realistic outcomes unique to each patient. Direct patient care or necessary medical procedures, such as medication administration, are required under a nursing care plan. Additionally, it includes recommending the patient or getting in touch with them for a follow-up and teaching and counseling the patient on ongoing health care. System for Nursing Interventions Classification (NIC) 
To give patients the right treatment, nurses might employ one of more than 550 nursing intervention labels. These interventions are grouped into seven categories or groupings of interventions following the Nursing Interventions Classification system. Interventions in Behavioural Nursing 
These are medical procedures aiming to help people become more socially responsible. In contrast, behavioral therapies concentrate on the patient's behavior, which is then expected to be improved. Several illustrations of behavioral nursing interventions include the following:
Nursing Interventions in the Community 
These initiatives demonstrate the community-wide strategy for promoting positive behavior change. In addition to focusing largely on the individual as a change agent, community interventionists are aware of a range of external circumstances that may impact a person's ability to achieve optimal health, such as:
Nursing interventions for families 
Health System Nursing Interventions
For to make a medical institution secure for all patients and staff, the following measures are taken:
Interventions in Physiology by Nurses 
These medical treatments check that a patient's physical needs are met and that they are healthy. These nursing interventions fall into two categories: 1) Basic and 2) Complex. 1) Basic Hands-on activities ranging from feeding to hygiene aid are considered basic interventions affecting the patient's physical health. 2) Complex Inserting an IV line to deliver fluids to a dehydrated patient is a more complicated physiological nursing intervention. Nursing Interventions for Safety The following actions are taken to safeguard patients and avoid harm:
Nursing Care Implementation Skills 
To properly carry out the care plan, nurses require cognitive, interpersonal, and technical abilities. 1) Cognitive: Cognitive capabilities include problem-solving, judgment, critical analysis, clinical reasoning, and creativity and before providing client care, cognitive skills, often called intellectual skills, require acquiring essential information, such as knowledge of the fundamental sciences and the logic behind nursing practices. 2) Interpersonal Skills: The ability to think, act, and relate to others is referred to as interpersonal ability. The nurse's ability to communicate with the patient and other healthcare team members is frequently a determining factor in the success of a nursing intervention. 3) Technical skills: Technical skills include deliberate "hands-on" abilities, including changing sterile dressings, injecting patients, operating machinery, bandaging, moving, lifting, and repositioning patients. All of these duties need to be completed efficiently and safely. Procedure for Implementation
The following are generally involved in the implementation process: 1) Re-evaluate the client Before putting one in place, the nurse must review the client to see whether the intervention is still necessary. The client's condition can have altered even though an order is listed on the care plan. 2) Determining whether the nurse needs Help Members of the healthcare team who are not registered nurses may also carry out additional nursing duties or activities. Along with certified healthcare professionals like licensed practical nurses and licensed vocational nurses (LPNs/LVNs), this team may comprise unlicensed assistive persons (UAP) and carers. When performing a nursing intervention, such as repositioning a client or ambulating an unstable obese client, the nurse may require help. 3) Implementing the nursing interventions into practice In addition to having a solid understanding of the sciences, nursing theory, nursing practice, and the ethical and legal implications of nursing interventions, nurses must also have the psychomotor skills necessary to carry out treatments safely. What interventions will be performed, what feelings to expect, what the client is asked to accomplish, and what the intended outcome is all need to be described, explained, and made clear to the client by the nurse. When giving care, nurses do duties that may be independent, dependent, or interdependent. Categories of Nursing Intervention
According to the function of the healthcare provider participating in the patient's care, nursing interventions are divided into three categories: 1) Personalized nursing interventions 
Without the aid or support of other medical staff, a registered nurse can carry out unilateral procedures such as: 2) Normal nurse duties like vital signs checks 
The process of informing a patient about the significance of their prescription so they can take it as directed 3) Dependent Nursing Interventions 
A nurse must start dependent interventions. A doctor or other medical expert must provide direction or supervision for some tasks, such as:
4) Nursing Interventions in Relationship 
A nurse participates in collaborative or interdependent interventions that include interdisciplinary teams of team members.
5. Evaluation
A successful patient outcome depends heavily on this latter stage of the nursing process and evaluation is the fifth stage of the nursing process. The team now assesses what works and what doesn't by reviewing what was done in the past after every nurse intervention activity has been performed. A healthcare practitioner must reassess or review each time they intervene or provide therapy to ensure the desired outcome. The three possible patient outcomes may be divided into three primary categories: improved, stable, and deteriorated health. 1) The Evaluation Process 
To determine if a care plan will be successful or unsuccessful, it is necessary to collect data, compare it to the targeted outcomes, analyze patient answers, continue, change, or end the nursing care plan, and plan for future nursing care. 2) Data Collection 
The nurse gathers information so that judgments regarding whether goals have been achieved may be made. It is frequently crucial to gather both objective and subjective data. Data must be written clearly and exactly to make the next step of the evaluation process easier. 3) Data comparison with desired results 
The client's progress is evaluated following the nursing care plan's specified goals and objectives when determining whether the anticipated outcome has been achieved or partially achieved.
4) Analyzing a PatientResponse to Nursing Interventions 
The nursing actions' impact on the results, including whether they were completed successfully, must also be established. 5) Identifying Elements That Affect Success or Failure 
More information must be gathered to determine whether the plan was successful. A variety of circumstances may influence the accomplishment of goals. For example, the client's family might or might not be supportive, and the client might or might not want to participate in such activities. 6) Nursing Care Plan: Continuation, Modification, or Termination 
Nursing is a dynamic, circular process. If the targets are unmet, the nursing process begins at step one. Depending on the overall patient status, they may need to be regularly revaluated and modified to be relevant. Depending on the findings of a new review, the treatment plan might need to be changed. Issues could develop or evolve in such a way. New targets are set when the clients reach their existing ones. If objectives are not fulfilled, nurses must assess why they are not being met and suggest changes to the nursing care plan. 7) Discharge Planning 
Transferring a patient from one level of care to the next is called discharge planning. Discharge plans are personalized instructions when the patient gets ready for independent living at home or continuous care outside the healthcare institution. A discharge plan's main objective is to raise the patient's quality of life by guaranteeing continuity of care and arranging for ongoing medical attention from other medical professionals or the patient's family.
Next TopicPeninsula Definition
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










