Osteoarthritis DefinitionOsteoarthritis (OA) is a kind of arthritis that affects the joints, particularly the weight-bearing joints such as the knees, hips, and spine, as well as the hands and feet. It is a chronic and progressive condition characterised by the slow deterioration of the cartilage that cushions the joints, resulting in pain, stiffness, and decreased mobility. 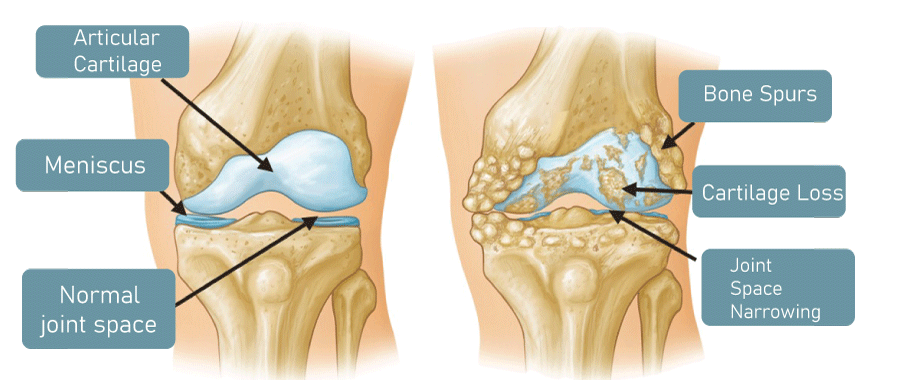
Cartilage is a form of connective tissue that covers the ends of bones and serves as a shock absorber when moving. In OA, the cartilage deteriorates and wears away over time, causing the bones to rub against one another and resulting in pain, inflammation, and bone damage. Although the illness can affect people of any age, elderly people are more likely to contract it. Major Causes of OsteoarthritisMillions of people worldwide suffer from osteoarthritis (OA), a prevalent degenerative joint disease. There are a number of factors that can contribute to the development of Osteoarthritis, even if its precise cause is not entirely understood. The following is a description of some of the major Osteoarthritis causes. AgeThe chance of developing Osteoarthritis increases significantly with age. As we become older, the cartilage that protects and cushions our joints deteriorates, making it more susceptible to injury, wear, and strain. A person's likelihood of acquiring OA increases as they age because the body becomes less capable of repairing damaged cartilage. GeneticsThe onset of Osteoarthritis may be influenced by genetics, according to some evidence. Specific genetic variations that affect the production and activity of enzymes required for cartilage repair and maintenance may have an impact on a person's susceptibility to cartilage damage and disintegration. Joint InjuryIt is more likely that a joint will develop Osteoarthritis if there has been prior damage to it, such as a ligament tear or fracture. It is possible for joint injury and cartilage breakdown to occur as a result of trauma to the cartilage or changes in the mechanics of the joint. Joint OveruseAnother factor in the onset of Osteoarthritis is the overuse of a joint repeatedly. This is particularly true for weight-bearing joints like the knees and hips, which experience continuous stress from exercises like jogging or jumping. Inflammation and cartilage deterioration can develop from microtrauma to joint tissues brought on by overuse. ObesityThe risk of OA is significantly increased by obesity, particularly in weight-bearing joints. The joints are put under additional strain from an excessive body weight, which damages the cartilage and speeds up wear and tear. A further association between obesity and persistent low-grade inflammation has been found, and this inflammation may play a role in joint deterioration and injury. Joint MisalignmentThe likelihood of developing Osteoarthritis may be increased by joint misalignment or the wrong way around which the bones are positioned in a joint. Bone misalignment can lead to an uneven distribution of load and tension on the joint surfaces, which can lead to cartilage deterioration and joint degeneration. Other Medical ConditionsOsteoarthritis development risk may be increased by some medical conditions. A secondary diagnosis of Osteoarthritis is more common in those with rheumatoid arthritis, a chronic autoimmune condition. Other medical conditions that can increase the risk of Osteoarthritis include congenital diseases like hip dysplasia and metabolic diseases like diabetes and gout. Hormonal ChangesOA may develop as a result of hormonal changes, particularly in women. Following menopause, the hormone oestrogen, which is crucial for bone health, decreases, which may hasten bone loss and cartilage deterioration. Environmental FactorsThe onset of Osteoarthritis may also be influenced by exposure to particular toxins or chemicals, for instance. For instance, lead and cadmium exposure?two heavy metals ubiquitous in various industrial settings?has been linked to a higher risk of OA. Common Symptoms Associated with OsteoarthritisA person's age, general health, and other characteristics, as well as the location and severity of the joint injury, can all affect how they feel when they have Osteoarthritis. Listed here are a few of the most typical Osteoarthritis symptoms. Joint PainA common indicator of Osteoarthritis is joint pain. The discomfort, which may be described as a dull ache or a sharp, stabbing sensation, might get worse during or right after physical exercise as well as during periods of inactivity. The painful joint may also be stiff or sensitive. Joint StiffnessJoint stiffness is a typical Osteoarthritis symptom. It may be more difficult to move the affected joint through its full range of motion in the morning or after periods of inactivity due to the stiffness. The stiffness may be accompanied by a tightness or tension in the joint. Joint TendernessJoint pain is a typical sign of Osteoarthritis, especially when the afflicted joint is touched or under pressure. Localised or widespread joint tenderness is possible. Reduced Flexibility and Range of MotionLoss of range of motion and flexibility in the affected joint can result from Osteoarthritis. Reaching and bending might become challenging as a result. The joint may feel tight or stiff as a result of the reduced range of motion. Swelling and InflammationThe common signs of Osteoarthritis include swelling and inflammation, particularly in the latter stages. There may only be swelling in the injured joint or it may be widespread. The joint may feel warm to the touch due to the inflammation, and the skin may become red or discoloured. Crunching or Popping SensationsWhen moving the painful joint, some Osteoarthritis sufferers may experience a crunching or popping sensation. Because of the loss of cartilage, the bones rub against one another, causing this. Bone Spurs or Bony GrowthsBony growths or spurs around the affected joint may develop as a result of Osteoarthritis in some cases. These growths may need to be surgically removed because they might add to joint pain and stiffness. Muscle WeaknessOsteoarthritis can result in muscle weakness in the affected joint due to decreased mobility and range of motion. As a result, some actions may be challenging to complete, and with time, the joint degeneration may worsen. Numbness or TinglingRarely, Osteoarthritis -related numbness or tingling may develop in the affected joint or nearby areas. An examination by a doctor is necessary because this can be a sign of nerve compression or injury. Diagnosis of OsteoarthritisDiagnosis of osteoarthritis typically involves a combination of patient history, physical examination, and diagnostic imaging. Patient HistoryOne of the first steps in diagnosing osteoarthritis is obtaining a detailed patient history. This involves asking the patient about their symptoms when they first began, and how they have progressed over time. The doctor will also ask about any previous injuries or surgeries to the affected joint, as well as any family history of joint disorders. It is important to understand the patient's medical history, as other medical conditions such as diabetes or obesity may affect the progression of osteoarthritis. Physical ExaminationA physical examination is usually the next step in diagnosing osteoarthritis. The doctor will examine the affected joint for signs of inflammation, such as redness, swelling, or warmth. They will also assess the joint's range of motion and perform tests to assess the joint's stability and strength. During the physical exam, the doctor may also test for the presence of joint crepitus, which is a popping or cracking sound that occurs with joint movement. Diagnostic ImagingIf osteoarthritis is suspected, the doctor may order diagnostic imaging tests to confirm the diagnosis. The most commonly used imaging tests include X-rays, MRI, and CT scans. X-raysX-rays are often the first imaging test ordered when osteoarthritis is suspected. X-rays are useful for detecting changes in the bones that occur with osteoarthritis, such as joint space narrowing, osteophyte formation, and subchondral sclerosis. X-rays can also be used to monitor the progression of osteoarthritis over time. MRIMRI is a more detailed imaging test that can detect changes in the soft tissues surrounding the joint, such as the cartilage and ligaments. MRI can also be used to identify early signs of osteoarthritis before they are visible on X-rays. CT ScansCT scans provide a detailed 3D image of the joint and can be used to detect bone spurs, cysts, and other abnormalities that may be contributing to osteoarthritis symptoms. Laboratory TestsIn some cases, the doctor may order laboratory tests to rule out other medical conditions that may be contributing to joint pain and stiffness. Blood tests may be ordered to test for rheumatoid factor or anti-CCP antibodies, which are indicators of autoimmune disorders such as rheumatoid arthritis. Blood tests may also be used to assess kidney and liver function, as some medications used to treat osteoarthritis can be hard on these organs. Joint Aspiration:In some cases, the doctor may perform a joint aspiration, which involves using a needle to withdraw fluid from the joint. The fluid can be tested for signs of infection or inflammation, and can also help relieve pain and swelling. Treatment of OsteoarthritisTreatment for osteoarthritis typically involves a combination of lifestyle changes, medications, and therapies. 1. Lifestyle ChangesLifestyle changes can be an effective way to manage the symptoms of osteoarthritis. The following lifestyle modifications may be recommended:
2. MedicationsSeveral medications can be used to manage the symptoms of osteoarthritis. These include:
3. TherapiesSeveral therapies can be used to manage the symptoms of osteoarthritis. These include:
ConclusionOsteoarthritis is a prevalent illness that results in stiffness and pain as joints degrade. It typically first manifests in middle age or later.Although there is presently no treatment, scientists are working to find ways to lessen or even undo the damage. Treatment options for managing pain include drugs, procedures, and lifestyle changes like stretching, exercise, and nutritional supplements.
Next TopicPancreas Definition
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share









