Sterilization DefinitionSterilization is used in healthcare institutions to eradicate or destroy all forms of microbial life, including fungi, bacteria, multicellular eukaryotic organisms, and other biological agents. 
Sterilization is carried out to stop the growth of microbes that may colonize an object's surface if the germs are not eradicated. Heat, sunlight, high pressure, radiation, filtration, & chemicals are just a few sterilization methods. Disinfection, sanitization, & pasteurization are different from sterilization in that they lessen rather than eliminate any living organisms or biological agents that could be present. A thing that has been sterilized is referred to as sterile or aseptic. Classification of SterilizationIn microbiology, sterilization can be accomplished using various physical and chemical techniques. Physical sterilization & chemical sterilization are the two categories under which sterilization is categorized. Let's go through them in more depth. Physical Sterilization MethodsThe following methods are included in physical sterilization: 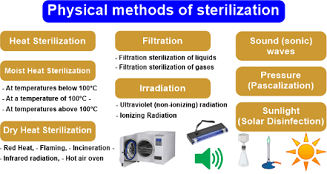
Heat SterilizationHeat sterilization is the most effective method of sterilization since it completely gets rid of bacteria by destroying their enzymes and cellular components. It is done using two techniques: 1. Wet Heat- It is one of the best sterilizing methods. An autoclave is used to carry out the moist heat sterilization process. Pressure-driven steam generation is the principle underlying how an autoclave works. Therefore, steam sterilization is another name for wet heat sterilization. Steam is often used in wet heat sterilization at temperatures between 121 to 134 °C. High pressure raises the boiling point of water, allowing for a greater temperature for sterilization. This approach is far more efficient than dry heat sterilization, which kills bacteria by oxidation. In this process, the microorganisms are destroyed by coagulating their proteins. It is used in the medical and pharmaceutical sectors to treat dirty and contaminated products and sterilize bandages, sheets, surgical & diagnostic types of equipment, containers, and more. 2. Dry Heat- It should be obvious from the name that the dry heat method doesn't need any water; hence hydrolysis won't occur here. The two best practices for using dry heat are flaming and baking. The oxidation of biological components kills bacteria using dry heat procedures. The material is heated since it takes more effort and energy than just breaking down proteins. When an autoclave is used, sterilization can be completed in about 15 minutes. However, dry heating necessitates sterilizing the item to 160 degrees Celsius. It's one of the most trustworthy sterilization procedures that is frequently used in sterilizing methods. The micro lab doesn't need a specialist to carry out this heating because it is the simplest method. Dry heat sterilization comes in a variety of forms, which are described below: Red Heat-
Flaming-
Incineration-
Hot air oven-
Infrared radiation-
FiltrationFiltration is distinct from other sterilizing methods in that it eliminates bacteria rather than removing them. However, cleaning the liquid takes more time. It may also clarify and sterilize liquids and gases since it can block the flow of both viable & nonviable particles. For the filtering procedure, there are several types of filters available. The most common filter types are
IrradiationTo sterilize surfaces and things, the process of irradiation involves exposing them to various radiation types. For sterilizing, electromagnetic radiation is mostly used.
Due to the low energy and low penetrating capacity of non-ionizing rays, UV rays have a wavelength between 260 and 280 nanometers. They are exposed to the material intoet rid of germs and other microbes. UV radiation is inappropriate for sterilizing pharmaceutical dosage forms due to its weak capacity to penetrate traditional packaging materials. Nevertheless, it is used to treat manufacturing-grade water, sterilize air, and sterilize the surfaces of aseptic work environments.
The two types of ionizing radiation most frequently used for sterilization are X and gamma rays. These are highly energetic radiations that ionize different substances, including water. A significant number of hazardous O2 metabolites, including the hydroxyl radical, superoxide ions, and H2O2, are produced through the ionization of water. These metabolites are strong oxidizers that destroy bacteria by different oxidizing parts of their cells.
High-speed electrons are accelerated in this technique using the cathode material. The electromagnetic beams are created to eliminate all types of bacteria, fungi, viruses, and other microorganisms. Cold sterilization is the term used to describe this method of eradicating microorganisms via radiation. Sunlight (Solar Disinfection)
Chemical Sterilization Method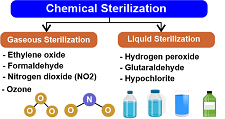
Chemicals are the everyday substances in a microbiology laboratory. While some chemicals have potentially harmful side effects, they work remarkably well to eradicate several unseen microorganisms. Chemical approaches have gained popularity since they are simple and cost-effective. Chemicals can eliminate harmful microorganisms from the surface by acting as disinfectants. Modern tools and devices used in hospitals and laboratories, like a a custom trayare frequently heat-sensitive. This indicates that they include some parts that should be protected from high temperatures. These components include rubber, glass, plastic, and other substances of the same kind. The option suggested is chemical sterilization, which may sterilize them without needing heat. Chemical sterilization can be done using liquid or gaseous chemicals.
It is possible to sterilize instruments chemically without heating them. But not all equipment and devices can be disinfected using this technique because some equipment or instruments include components that may react strongly with chemicals. It is advised that you read the manufacturer's instructions from the makers of the chemicals and the equipment to be sterilized before utilizing a chemical sterilization technique with these kinds of devices. Advantages and Disadvantages of SterilizationAdvantages-
Disadvantages-
The ConclusionSterilization is an essential procedure. It has a significant role in surgical management's success. However, alternative techniques are also employed for heat-sensitive products. Overall, heat sterilization is the best way. Boiling destroys the majority of vegetative cells but not bacterial spores. In comparison to moist heat, dry heat takes longer to kill organisms.
Next TopicTourism Definition
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










