Pancreas DefinitionThe pancreas is a six-inch-long abdominal gland. It has a flat pear shape and is encircled by the liver, spleen, gallbladder, small intestine, stomach, and gallbladder. The metabolism of essential molecules that provide cells with energy is dependent on an organ known as the pancreas. To guarantee optimal pancreas function for many years, even young and healthy individuals should maintain a nourishing diet and a proper way of life. Functions of PancreasThe pancreas is a vital organ that serves a number of vital roles in the human body. A duct connects it to the small intestine and is situated behind the stomach. Exocrine and endocrine are the pancreas' two primary activities. 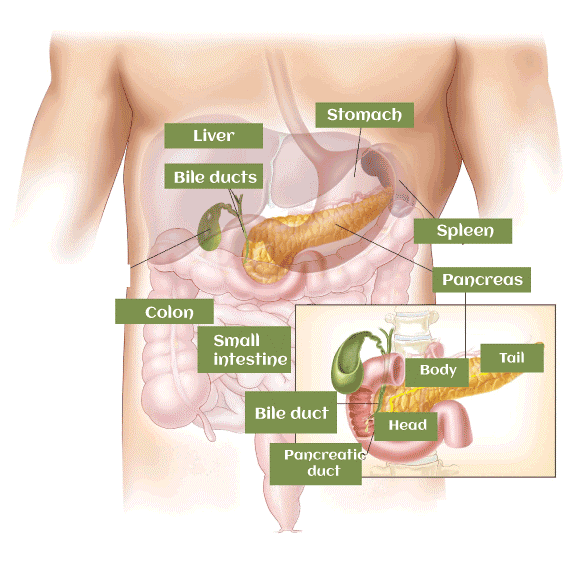
Exocrine FunctionThe pancreas performs its exocrine function by secreting digestive enzymes and bicarbonate into the small intestine. Digestion enzymes break down proteins, lipids, and carbohydrates in food into smaller molecules that can be easily absorbed by the body. By making the stomach's acidic environment more alkaline and creating an ideal setting for the digestive enzymes to function, the bicarbonate contributes to neutralising the acidic environment. In addition to amylase, lipase, and protease, the pancreas also secretes other digesting enzymes. Proteins are broken down by protease, carbohydrates by lipase, and lipids by amylase. When required, these enzymes are activated in the small intestine after being created in the pancreas in an inactive state to protect the organ. Endocrine FunctionSecretion of hormones that control blood sugar levels in the body is a part of the pancreas' endocrine function. Insulin and glucagon are the main hormones produced by the islets of Langerhans, a group of cells located in the pancreas. When blood sugar levels are high, the hormone insulin is released, which helps in the uptake of glucose into cells and lowers blood sugar levels. Somatostatin and pancreatic polypeptide are some of the other hormones the pancreas makes. Somatostatin prevents the release of glucagon and insulin, and pancreatic polypeptide aids in controlling hunger and digestion. During a regular meal, food travels from the mouth to the stomach through the oesophagus. Food is broken down by digestive acids in the stomach. Direct entry of the partially digested food into the "duodenum," the first part of the small intestine. The duodenum is where pancreatic and hepatic bile enters the digestive tract. The duodenum connects to the remaining sections of the small bowel, where food is further digested, and from there to the large intestine, also known as the colon, where the fully digested material exits the body through the anus. How Does Pancreas Help in Digestion?The digestive enzymes are created by the exocrine cells of the pancreas. Pancreatic enzymes are released into a network of tiny ducts that branch out from the main pancreatic duct by exocrine cells in the pancreas when food enters the stomach. Pancreatic juice, which is comprised of secretions and pancreatic enzymes, is transported down the pancreatic duct, which spans the whole length of the organ. At the ampulla of Vater, the main pancreatic duct joins the common bile duct, and the two organs then travel together to the duodenum. Bile is released from the gallbladder via the common bile duct. To aid in the digestion of fats, carbohydrates, and proteins, bile and pancreatic enzymes now move to the duodenum. Helps in Blood Sugar Regulation The cells that produce hormones in the pancreas are called endocrine cells. Specific physiological functions are controlled by substances known as hormones. The majority of the time, they begin in one area of the body and spread to another through the blood. Insulin and glucagon are the two main hormones produced by the pancreas. Endocrine cells called pancreatic islet cells produce and release the chemicals insulin and glucagon into circulation. Glucagon lowers blood sugar levels as opposed to insulin. These two major hormones function in concert to keep the right blood sugar level. Different Parts of the Pancreas 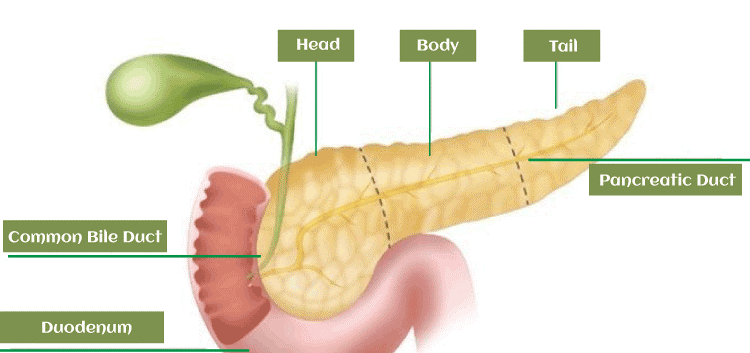
Hormones secreted by Pancreas
How to keep the pancreas healthy?
Conditions Affecting PancreasDiabetes mellitus is one of the most well-known conditions brought on by an endocrine system that isn't functioning properly. It's possible for people with some types of diabetes to not create enough insulin in their pancreas to keep their blood sugar levels stable. Some of its symptoms are
The pancreas is a vital organ that plays a critical role in digestion and the regulation of blood sugar levels. When the pancreas fails to function properly, it can lead to a range of disorders, which can be life-threatening if left untreated. Here are some of the major diseases related to the pancreas. PancreatitisAn inflammation of the pancreas known as pancreatitis can result in vomiting, nausea, and excruciating abdominal pain. Acute or chronic forms of this illness are both serious and potentially fatal, with acute being more severe. Gallstones, drinking excessively, or having high triglyceride levels in the blood are the usual causes of acute pancreatitis. Long-term alcohol misuse is frequently linked to chronic pancreatitis, but cystic fibrosis and hereditary conditions can also be to blame. Hospitalisation, pain medication, and intravenous hydration fluids may all be used as pancreatitis treatments. Surgery can be necessary to remove the gallstones, for example, if the underlying cause of pancreatitis is found. A portion of the pancreas may need to be surgically removed in extreme circumstances. Pancreatic CancerAn instance of pancreatic cancer typically develops in the cells that make digestive enzymes and damages the pancreas.Since symptoms of this cancer may not appear until it has spread to other body parts, it is frequently discovered when it is already advanced. Jaundice, stomach pain, unexplained weight loss, and appetite loss are all indications of pancreatic cancer. Although the exact causes of pancreatic cancer are unknown, risk factors include smoking, being overweight, having a family history of the disease, and being exposed to certain chemicals. According to the cancer's stage and location, treatment options for pancreatic cancer frequently include surgery, chemotherapy, or radiation therapy. DiabetesHigh blood sugar levels are a hallmark of diabetes, a metabolic illness. Insulin, a hormone made by the pancreas, permits cells to take up glucose from the bloodstream, assisting in the regulation of blood sugar levels. The pancreas either produces insufficient amounts of insulin in diabetics, or the body develops a resistance to insulin's effects. Type 1, type 2, and gestational diabetes are a few of the several kinds of the disease. The immune system of the body targets and kills the insulin-producing cells in the pancreas, resulting in type 1 diabetes, an autoimmune illness. When the body develops an insulin resistance or the pancreas produces insufficient insulin, type 2 diabetes, which is more prevalent, results. Pregnancy difficulties for both the mother and the unborn child are increased by gestational diabetes. Dietary modifications, physical activity, and medications to help control blood sugar levels are frequently part of diabetic treatment. Cystic FibrosisThe pancreas, the digestive system, and the lungs are all impacted by the hereditary condition known as cystic fibrosis. People who have cystic fibrosis have a defective gene that results in the production of thick, sticky mucus, which can obstruct the pancreatic ducts and clog the airways. As a result, the pancreas may eventually become damaged and develop chronic pancreatitis. In addition to frequent lung infections, abdominal pain, bloating, and poor weight gain, cystic fibrosis symptoms can include continuous coughing, wheezing, and digestive issues. Nutritional supplements, pancreatic enzyme replacement therapy, and drugs to help the lungs function better are all possible treatments for cystic fibrosis. Pancreatic DivisumWhen the ducts that drain the pancreas do not properly merge during foetal development, a congenital disease known as pancreatic divisum results. Digestive enzymes may build up in the pancreas as a result of this, which over time may inflame and harm the organ. Abdominal pain, nausea, and vomiting are pancreatic divisum symptoms. Endoscopic therapy may be used as a form of treatment to expand the ducts and enhance drainage. Zollinger-Ellison SyndromeWhen tumours form in the pancreas or duodenum and release an excessive amount of the hormone gastrin, the condition known as Zollinger-Ellison syndrome develops. This hormone increases the formation of stomach acid, which can cause peptic ulcers and other gastrointestinal issues. Abdominal pain, diarrhoea, and weight loss are Zollinger-Ellison syndrome symptoms. Surgery to remove the tumours or medicines to lower the production of stomach acid may be used as treatments. Autoimmune PancreatitisRarely, autoimmune pancreatitis develops when the pancreas is unintentionally attacked by the immune system. Over time, this may cause injury, inflammation, and scarring. Jaundice, weight loss, and stomach pain are all signs of autoimmune pancreatitis. To reduce inflammation and inhibit the immune system, corticosteroids may be used as a form of treatment. Pancreatic PseudocystsFluid-filled sacs called pancreatic pseudocysts can develop in the pancreas as a result of acute pancreatitis or other pancreatic injuries. Although some of these cysts may go away on their own, larger or persistent cysts might need to be surgically removed. Abdominal pain, nauseousness, and vomiting are signs of pancreatic pseudocysts. Life Without PancreasPatients with chronic pancreatitis, newly forming tumours (like adenocarcinoma, neuroendocrine tumours, duodenal cancer, or lymphoma), and hyperinsulinemic hypoglycemia (a condition where high levels of insulin cause a drop in blood sugar levels) may require surgical removal of the pancreas (pancreatectomy). The surgeon may also remove the spleen, a portion of the stomach, the gallbladder, and a portion of the bile ducts in addition to the duodenal intestine (the first part of the small intestine), as the pancreas is surrounded by other organs. Living without a pancreas is possible, but it requires some major adaptations. Tragically, after surgery to remove this gland, it is necessary to take drugs continuously, including those that substitute for pancreatic enzymes and insulin, and it is also crucial to entirely change the diet.
Next TopicParadox Definition
|
 For Videos Join Our Youtube Channel: Join Now
For Videos Join Our Youtube Channel: Join Now
Feedback
- Send your Feedback to [email protected]
Help Others, Please Share










